Infectious disease specialist
Sinitsyn
Olga Valentinovna
33 years of experience
Highest qualification category of infectious disease doctor
Make an appointment
Hemorrhagic fever with renal syndrome (another name is mouse fever) is an infectious disease, often associated with the beginning of the summer season and agricultural work. Every year, about 7,000 cases of infection are registered in the country, which makes itself felt with characteristic symptoms - hemorrhagic rash, vascular damage, kidney failure and a general deterioration in a person’s condition. In the absence of timely help, the disease can cause serious complications and death. Only timely seeking medical help will help maintain the patient’s health and return him to normal life.
General information
Murine fever is often called hemorrhagic fever with renal syndrome (HFRS) . This is an acute viral disease of a zoonotic nature (the source of infection is animals), which spreads in a certain area. Hemorrhagic mouse fever begins acutely. As the disease develops, blood vessels are affected, hemorrhagic syndrome , severe kidney damage and general intoxication of the body .
Hemorrhagic fever is a serious disease that requires adequate and timely treatment. Otherwise, severe kidney damage can lead to serious complications and even death. The carriers of infection in nature are mouse-like rodents. As Wikipedia and other sources indicate, an increase in incidence is observed in the summer and autumn, although cases of mouse fever are diagnosed throughout the year. A person can become infected by inhaling dust contaminated with the virus, as well as by consuming water and food contaminated with secretions of mouse-like rodents. There is no transmission of the disease from person to person. Sporadic cases of the disease, as well as epidemic outbreaks, are recorded. It has been noted that HFRS most often develops in men, since infection often occurs during agricultural work, during hunting, fishing, etc. People of working age are predominantly affected.
This article will discuss how to recognize the symptoms of this disease, as well as the features of its treatment.
Treatment process
Treatment of the disease, both in children and men, is carried out in the infectious diseases department of the hospital. During treatment, a number of laboratory procedures are prescribed, including blood and urine tests, PCR, and coagulogram. The patient is prescribed bed rest from 1 week to 1 month. Treatment consists of the use of antipyretic, analgesic and antiviral drugs, anti-inflammatory drugs, etc. In addition to all treatment, infusion therapy is prescribed, and glucocorticoids are prescribed as medications.
Treatment with anticoagulants is applicable for thrombotic-coagulation syndrome. In parallel with the procedure, a course of vitamins is prescribed.
Pathogenesis
The causative agent of mouse fever is a virus that belongs to the Bunyaviridae family. It belongs to an independent genus – Hantavirus. The virus replicates in the cytoplasm of infected cells. In the external environment, it is relatively stable at temperatures from 4 to 20 degrees. The virus is completely inactivated at a pH below 5.0; it is sensitive to chloroform , ether , acetone , ultraviolet , benzene .
The sources of the disease are only about sixty animal species. But the main distributors of the virus are field mice, gray and black rats, and different types of voles.
Through the upper respiratory tract, the pathogen enters the human lungs, after which it is disseminated to other organs through the blood. Once in the human body, the virus gradually migrates and is localized in the vascular endothelium and epithelial cells of various organs. Gradually it accumulates and replicates in the vascular epithelium. When the viremia phase begins, symptoms of intoxication and other signs of the disease appear.
The virus has a toxic effect on blood vessels, provoking the development of destructive arteritis with increased permeability of the vascular wall. Microcirculation is disrupted, as the vegetative centers that determine it are affected. DIC syndrome and multiple organ failure develop.
The virus has a pronounced negative effect on the condition of the kidneys. Their size increases significantly, and the capsule is tense. Necrosis and hemorrhages in the cortical layer are detected
Severe serous-hemorrhagic apoplexy is observed in the medulla. infarctions may occur . Due to massive desquamation of the epithelium and fibrin deposition in the tubules, obstructive segmental hydronephrosis .
During the development of the disease, pathomorphological changes occur in other organs. Hemorrhages, plethora, dystrophy, necrosis, and edema are possible.
Characteristics of the causative agent of hemorrhagic fever with renal syndrome
The causative agent of HFRS, a virus, was isolated by South Korean scientist HWLee from the lungs of a rodent. The virus was named Hantaan (after the Hantaan River, which flows on the Korean Peninsula). Later, such viruses were discovered in many countries - in Finland, the USA, Russia, China and others. The causative agent of HFRS is classified in the bunyavirus family (Bunyaviridae) and is classified into a separate genus, which includes several serovars: the Puumala virus circulating in Europe (epidemic nephropathy), the Dubrava virus (in the Balkans) and the Seul virus (distributed on all continents). These are RNA-containing viruses up to 110 nm in size, they die at a temperature of 50 ° C for 30 minutes, and at 0-4 ° C (the temperature of a household refrigerator) they persist for 12 hours.
There are two types of HFRS virus: type 1 – eastern (common in the Far East), the reservoir is the field mouse. The virus is highly variable and can cause severe forms of infection with a mortality rate of up to 10-20%. Type 2 – western (circulates in the European part of Russia), reservoir – bank vole. Causes milder forms of the disease with a mortality rate of no more than 2%.
Classification
Depending on the severity of intoxication, hemorrhagic and renal syndromes, the tactics of the disease are distinguished:
- Mild - fever lasts up to 5 days, the temperature does not rise above low-grade levels, diuresis decreases slightly (750-1000 ml of urine per day), a mild rash on the skin and mucous membranes, and short-term headaches are noted.
- Moderate - begins acutely, fever lasts up to 7 days, moderate intoxication is noted, temperature can rise above 39 degrees. Hemorrhagic syndrome is clearly defined - there is a rash on the skin, hemorrhages at the injection sites, hemorrhages in the sclera, conjunctiva. Oligouria and hyperazotemia are characteristic.
- Severe – severe intoxication is noted, the temperature rises above 39.5 degrees. Hemorrhagic syndrome is pronounced - hemorrhages are observed on the skin and mucous membranes, bleeding from internal organs, and profuse nosebleeds occur. Characterized by oligoanuria or anuria , cylindruria , significant proteinuria , hematuria , severe hyperazotemia .
CHILD WITH FEVER
Fever is the most common symptom of illness in children: every child suffers from a febrile illness at least once a year. But they also represent the most common reason for the use of medications: almost all children with fever receive antipyretics even at a low temperature - below 38°. This is facilitated by the idea that parents still have about the extreme danger of high temperature. As, indeed, is the doctor’s desire to alleviate the discomfort associated with temperature, or at least prescribe treatment, the effect of which will be obvious.
Mass consumption of antipyretics imposes special requirements on their safety due to the possible development of complications in children. The fight against elevated temperature is an important element in the treatment of many diseases, but it cannot be considered an end in itself: after all, by lowering the temperature, in most cases we do not affect the course and severity of the disease. Therefore, those doctors and parents who strive at all costs, by any means, to reduce the temperature of a sick child and keep it at normal values are wrong: such behavior indicates their poor knowledge of the causes and role of fever.
First of all, about the normal body temperature of the child. It is not 36.6°, as many believe, but fluctuates during the day by 0.5°, in some children - by 1.0°, increasing in the evening. When measuring the temperature in the armpit, a value of 36.5–37.5° can be considered normal: the maximum temperature (rectal) averages 37.6°, exceeding 37.8° in half of the children [1]. Axillary temperature is 0.5–0.6° lower than rectal temperature, but there is no exact conversion formula; It is important to remember that a temperature above 38°, wherever it is measured, in most children (including the first months of life) corresponds to febrile temperature, and the difference in tenths of a degree does not matter much. But there is no reason to worry if a child’s temperature (in the absence of other symptoms) “jumps” to 37.3–37.5° in the evening; By the way, the temperature decreases somewhat if you let the child cool down before measuring.
Regulation of body temperature is achieved through the balance of heat production and heat transfer. The body generates heat by burning (oxidizing) carbohydrates and fats in tissues, especially when muscles work. Heat is lost as the skin cools; its losses increase with the dilation of skin vessels and evaporation of sweat. All these processes are regulated by the hypothalamic thermoregulatory center, which determines the amount of heat production and heat transfer.
Fever is a consequence of the action of endogenous pyrogens on the thermoregulatory center: cytokines, which are also involved in immunological reactions. These are interleukins IL-1 and IL-6, tumor necrosis factor (TNF), ciliary neurotropic factor (CNTF) and interferon-a (IF-a). Increased synthesis of cytokines occurs under the influence of products secreted by microorganisms, as well as by body cells when they are infected with viruses, during inflammation, and tissue breakdown. Cytokines stimulate the production of prostaglandin E2, which, as it were, moves the setting of the “central thermostat” to a higher level, so that normal body temperature is determined by it as lower. An increase in heat production due to increased muscle activity and trembling is accompanied by a decrease in heat transfer due to constriction of skin blood vessels. We perceive shivering and a feeling of cold (chills) as a “cold”; upon reaching a new temperature level, heat transfer increases (feeling of heat). Prostaglandin E2 can cause the muscle and joint pain we experience as aching during an acute infection, and IL-1 causes the drowsiness often seen in a child with a fever.
The biological significance of fever is protection against infection: animal models have shown an increase in infection mortality when fever is suppressed, and a similar effect has been described in humans [2]. Under the influence of moderate fever, the synthesis of interferons and TNF increases, the bactericidal capacity of polynuclear cells and the reaction of lymphocytes to mitogen increases, and the level of iron and zinc in the blood decreases. “Feverish” cytokines increase the synthesis of proteins in the acute phase of inflammation and stimulate leukocytosis. In general, the effect of temperature stimulates the type 1 T-helper immune response, which is necessary for adequate production of IgG antibodies and memory cells. Many microbes and viruses have a reduced ability to reproduce when the temperature rises.
Antipyretics lower the temperature without affecting the cause that caused it. In case of infections, they only transfer the setting of the “central thermostat” to a lower level, without reducing the total duration of the febrile period; but at the same time, the period of virus isolation is clearly prolonged, in particular in acute respiratory infections [3–5]. A direct inhibitory effect of these drugs on TNF-a production and anti-infective defense has been shown [6].
These and other similar data make us cautious about suppressing fever in infectious diseases; One should also take into account the fact that suppression of the production of interferon and IL-2 reduces the strength of the humoral immune response. This makes it plausible to assume that frequent acute respiratory viral infections in children are related to the widespread use of antipyretic drugs in our time; This may also be responsible for the upward trend in allergic diseases.
Another danger arises when using antipyretics. In most acute respiratory viral infections, the temperature lasts only 2–3 days, while in bacterial acute respiratory infections (otitis media, pneumonia) it lasts 3–4 days or more, which is often the only indication for prescribing antibiotics. The use of antipyretic drugs in such patients, especially the “course”, with suppression of temperature, creates the illusion of well-being, and by the end of the week it is necessary to take “heroic measures” to save the child’s life as a result of an advanced process. Therefore, to reduce the temperature you need to have sufficient reasons, and in any case you cannot try to prevent it from rising again.
Of course, closer to 40.0°, the protective functions of fever turn into the exact opposite: metabolism and O2 consumption increase, fluid loss increases, and additional stress is created on the heart and lungs. A normally developing child copes with this easily, experiencing only discomfort, but in patients with chronic pathology, fever can cause a deterioration in the condition. In particular, in children with damage to the central nervous system, fever contributes to the development of cerebral edema and seizures. Fever is more dangerous for children 0–3 months old. And yet, the dangers associated with an increase in temperature are largely exaggerated; in most infections, its maximum values do not reach 39.5–40.0°C, and there is no threat of developing persistent health disorders.
A study of the practice of using antipyretics showed that, for example, for ARVI, they are prescribed to 95% of sick children, even at temperatures below 38° (93%) [7]. Familiarizing pediatricians with modern approaches to this problem makes it possible to reduce the use of these drugs by 2–4 times.
The main febrile syndromes in children are associated with infection and are usually accompanied by quite distinct symptoms that allow at least a presumptive diagnosis to be made right at the patient’s bedside. The following list shows the main symptoms most often associated with high fever in children and the most common causes of their occurrence.
- Fever + rash in the early stages: scarlet fever, rubella, meningococcemia, allergic rash to an antipyretic drug.
- Fever + catarrhal syndrome from the respiratory system: ARVI - rhinitis, pharyngitis, bronchitis, possibly also bacterial inflammation of the middle ear, sinusitis, pneumonia.
- Fever + acute tonsillitis (tonsillitis): viral tonsillitis, infectious mononucleosis (Epstein-Barr virus infection), streptococcal tonsillitis or scarlet fever.
- Fever + difficulty breathing: laryngitis, croup (inspiratory shortness of breath), bronchiolitis, obstructive bronchitis, asthma attack due to ARVI (expiratory shortness of breath), severe, complicated pneumonia (groaning, groaning breathing, pain when breathing).
- Fever + cerebral symptoms: febrile convulsions (convulsive syndrome), meningitis (headache, vomiting, stiff neck), encephalitis (disorders of consciousness, focal symptoms).
- Fever + diarrhea: acute intestinal infection (usually rotavirus).
- Fever accompanied by abdominal pain and vomiting: appendicitis, urinary tract infection.
- Fever + dysuric symptoms: urinary tract infection (usually cystitis).
- Fever + joint damage: rheumatism, arthritis, urticaria.
- Fever + symptoms of very severe illness (“toxic” or “septic”); the condition requires immediate hospitalization and emergency intensive care, along with deciphering the diagnosis. These symptoms include:
- a sharp violation of the general condition;
- drowsiness (sleeping longer than usual or at unusual times);
- irritability (screaming even when touched);
- disturbance of consciousness;
- reluctance to take liquids;
- hypo- or hyperventilation;
- peripheral cyanosis.
With syndromes 1–9, diagnostic difficulties may, of course, occur, but the most important thing is to make an assumption about the most likely etiology of the process. Fever in a child 0–3 months of age may be a manifestation of a severe infection; in these cases, hospital observation is usually indicated. Long-term (more than 2 weeks) fever of unknown cause requires examination for long-term infection (sepsis, yersiniosis), connective tissue disease, immunodeficiency, and malignant pathology.
If a bacterial disease is suspected, an antibiotic should be prescribed, if possible without antipyretics, since they can mask the lack of effect of antibacterial treatment.
Fever without a visible source of infection (FWF) . Almost every child is examined for a febrile illness in the first 3 years of life. Of these, every fifth person does not reveal signs of a specific disease during examination [8]. Currently, such fever is considered as a separate diagnostic category. This refers to an acute illness manifested only by febrile fever in the absence of symptoms that would indicate a specific disease or source of infection. LBI criteria are a temperature above 39° in a child aged 3 months to 3 years and above 38° in a child 0–2 months of age in the absence of the above “toxic” or “septic” symptoms of a very serious disease at the time of the first examination.
Thus, the group of LBI includes children in whom febrile fever is detected against the background of a slightly disturbed general condition. The point of identifying the group of infectious diseases is that, along with non-life-threatening infections (enteroviral, herpetic types 6 and 7, etc.), it includes many cases of influenza, as well as latent (occult) bacteremia, i.e. e. the initial phase of a severe bacterial infection (SBI) - pneumonia, meningitis, pyelonephritis, osteomyelitis, sepsis, in which clinical symptoms may not occur at an early stage, providing a real opportunity to prescribe an antibiotic, preventing its progression.
The causative agent of occult bacteremia in 80% of cases is pneumococcus, less often - H. influenzae type b, meningococcus, salmonella. In children 0–2 months, Escherichia coli, Klebsiella, group B streptococci, Enterobacteriaceae, and Enterococci predominate. The frequency of occult bacteremia in children 3–36 months with LBI is 3–8% [9], at temperatures above 40°C - 11.6% [10]. In children 0–3 months of age with LBI, the probability of bacteremia or TBI is 5.4–22% [11, 12].
TBI does not develop in all cases of occult bacteremia; its frequency varies depending on the causative agent. Meningitis occurs in 3–6% of cases with pneumococcal bacteremia [13], but 12 times more often with hemophilus influenzae [14]. Urinary tract infection is detected in 6–8% of children, and in girls - up to 16% [15].
Neither the severity of clinical symptoms, nor high temperatures (above 40.0°), nor the lack of response to antipyretics allows for a reliable diagnosis of bacteremia, although they may indicate its increased likelihood. On the contrary, in the presence of leukocytosis above 15x109/l, as well as the absolute number of neutrophils above 10x109/l, the risk of bacteremia increases to 10–16%; less significant is the increase in the proportion of neutrophils above 60% [16–18]. But the absence of these signs does not exclude the presence of bacteremia, since every fifth child with bacteremia has a leukocytosis below 15x109/l [19].
The level of C-reactive protein (CRP) is more informative - 79% of children with bacteremia have numbers above 70 mg/l, while with viral infections only 9% [20], however, on days 1–2 of infection, CRP may still remain low . Blood culture to detect bacteremia is available only in the hospital; it takes about a day to obtain its results, so the influence of this method on the choice of treatment tactics is small. On the contrary, given the high incidence of urinary tract infections, urine cultures are highly advisable, especially since clinical urinalysis results are often negative.
In children without respiratory symptoms, bacterial pneumonia is rarely diagnosed, but with leukocytosis above 15x109/l, the presence of shortness of breath (>60 per minute in children 0–2 months, >50 in children 3–12 months and >40 in children over 1 year) and fever for more than 3 days, a chest x-ray often reveals pneumonia [21].
Febrile seizures - observed in 2-4% of children, most often between 12 and 18 months, usually with a rapid rise in temperature to 38° and above, but can also occur when it decreases. Their criteria are:
- age up to 6 years;
- absence of central nervous system disease or acute metabolic disorder that can cause seizures;
- no history of afebrile seizures.
Simple (benign) febrile convulsions do not last more than 15 minutes in duration (if they are serial, then 30 minutes) and are not focal. Complex seizures last more than 15 minutes (serial - more than 30 minutes - febrile status epilepticus), or are characterized by focality, or end in paresis.
Seizures occur more frequently with viral than with bacterial infections, and the most common cause is herpesvirus type 6, which accounts for 13–33% of initial episodes. The risk of developing febrile seizures after administration of DPT (on day 1) and viral vaccines (measles-rubella-mumps - on days 8-15) is increased, but the prognosis for children with these seizures did not differ from that for children with febrile seizures during infection.
The tendency to febrile seizures is associated with several loci (8q13-21, 19p, 2q23-24, 5q14-15), the nature of heredity is autosomal dominant. Most often, simple - generalized tonic and clonic-tonic convulsions lasting 2 - 5 minutes are observed, but atonic and tonic seizures can also occur. The facial and respiratory muscles are usually involved. Prolonged seizures are observed in 10% of children, focal seizures are observed in less than 5%; Although complex seizures may follow simple seizures, most children with complex seizures develop them on the first episode. Most often, seizures appear at the very beginning of the disease at a temperature of 38–39°, but repeated seizures can develop at other temperatures.
In a child with febrile seizures, meningitis should be ruled out first, and lumbar puncture is indicated if appropriate signs are present. Calcium testing is indicated in infants with signs of rickets to exclude spasmophilia. Electroencephalography is indicated after the first episode only for prolonged (>15 minutes), repeated or focal seizures, in which signs characteristic of epilepsy are sometimes revealed.
Rules for reducing temperature
Fever itself is not an absolute indication for lowering the temperature; in most infections, the maximum temperature rarely exceeds 39.5°, which does not pose any threat to a child older than 2–3 months. In cases where a decrease in temperature is necessary, it is not necessary to achieve normal values; it is usually enough to lower it by 1–1.5°, which is accompanied by an improvement in the child’s well-being. A child with a high fever should be given enough fluids, uncovered, and wiped with water at room temperature, which is often sufficient to reduce the temperature.
Consensus indications for reducing fever with antipyretics are [22]:
- In previously healthy children over 3 months of age: - temperature >39.0°, and/or - muscle aches, headache, - shock.
- In children with a history of febrile seizures - >38–38.5°.
- In children with severe diseases of the heart, lungs, and central nervous system - >38.5°.
- In children during the first 3 months of life - >38°.
Antipyretics are required, along with other measures (rubbing the skin, administering antiplatelet agents into a vein), in case of the development of malignant hyperthermia associated with impaired microcirculation.
Antipyretics should not be prescribed for a regular “course” of taking several times a day, regardless of the temperature level, since this sharply changes the temperature curve, which can make it difficult to diagnose a bacterial infection. The next dose of antipyretic should be given only after the child’s body temperature has returned to its previous level.
Selection of antipyretics
Antipyretics are the most widely used drugs in children, and they should be chosen primarily based on safety considerations rather than effectiveness. Numerous advertising publications emphasize the more pronounced antipyretic effect of this or that drug compared to paracetamol. This formulation of the question is inappropriate - we should be talking about the equivalence of doses and the ratio of the effectiveness and safety of the drug, and quickly reducing the temperature with the help of modern means to any level is not difficult. It is important to remember that drugs with a strong effect are more toxic, moreover, they often cause hypothermia with a temperature below 34.5–35.5 ° and a state close to collapse.
When choosing an antipyretic drug for a child, one should, along with the safety of the drug, take into account the convenience of its use, i.e., the availability of children's dosage forms and fractional dosages for different age groups. The cost of the drug also plays an important role.
The drug of first choice is paracetamol (acetaminophen, Tylenol, Panadol, Prodol, Calpol, etc.) in a single dose of 10–15 mg/kg (up to 60 mg/kg/day) [22]. It has only a central antipyretic and moderate analgesic effect, does not affect the hemocoagulation system and, unlike nonsteroidal anti-inflammatory drugs (NSAIDs), does not cause adverse reactions from the stomach. Taking into account the possible insufficient reduction in temperature at a dose of 10 mg/kg (which can lead to an overdose with repeated doses), it is recommended to use a single dose of 15 mg/kg when administered orally. Of the dosage forms of paracetamol in children, solutions are preferred - syrups, effervescent powders and tablets for preparing solutions, the effect of which occurs within 30 - 60 minutes and lasts 2-4 hours. Paracetamol in suppositories has a longer effect, but its effect occurs later. A single dose of paracetamol in suppositories can be up to 20 mg/kg, since the peak concentration of the drug in the blood reaches only the lower limit of the therapeutic range. Its effect occurs after approximately 3 hours [23, 24]. Paracetamol (Tylenol, Panadol, Prodol, Calpol, etc.) in children's forms is produced by many manufacturers; it is part of Cefekon-P suppositories. All these forms, and in dosages for children of any age, are available in the drug Efferalgan UPSA; they do not contain allergenic additives, and the solutions can be added to infant formulas and juices. Efferalgan syrup is equipped with a measuring spoon for precise dosing and is intended for children 1 month–12 years old weighing 4–32 kg (dosage is indicated taking into account differences of 2 kg).
Ibuprofen is a drug from the NSAID group, which, in addition to the central one, also has a peripheral anti-inflammatory effect; it is used in a dose of 6–10 mg/kg (daily dose, according to various sources, 20–40 mg/kg), which is comparable in effect to the above doses of paracetamol. Given this fact, WHO did not include ibuprofen in the list of essential medications. Moreover, ibuprofen produces more side effects (dyspeptic, gastric bleeding, decreased renal blood flow, etc.) than paracetamol - 20% versus 6% in large series of observations [25 - 27]. A number of national pediatric societies recommend the use of ibuprofen as a second-choice antipyretic in the following situations:
- for infections with a pronounced inflammatory component;
- in cases where fever in children is accompanied by pain reactions.
Ibuprofen is also available for children (ibufen, nurofen for children - syrup 100 mg in 5 ml); the tablet form of the drug (200–600 mg) is not suitable for this purpose.
In children during the first 3 months of life, both drugs are used in smaller doses and with a smaller frequency of administration.
Rubbing with water at room temperature provides an antipyretic effect during febrile conditions, although less pronounced than during heat shock (overheating) [28]. It is especially indicated for overly wrapped children, in whom decreased heat transfer aggravates the febrile state.
Drugs that are not recommended for use in children as antipyretics
Amidopyrine, antipyrine, and phenacetin were excluded from the list of antipyretics. However, in Russia, unfortunately, suppositories cefekon with phenacetin and cefekon M with amidopyrine continue to be used in children.
Acetylsalicylic acid in children with influenza, ARVI and chickenpox can cause Reye's syndrome - a severe encephalopathy with liver failure and a mortality rate above 50% [29, 30]. This served as the basis for a ban on the use of acetylsalicylic acid in children under 15 years of age with acute illnesses in most countries of the world (this ban has been in effect since the early 80s), as well as for mandatory appropriate labeling of drugs containing acetylsalicylic acid. Unfortunately, these rules are not followed in Russia. And Cefekon M and Cefekon suppositories containing salicylamide (a derivative of acetylsalicylic acid) in Moscow were included in the list of free prescription drugs.
Metamizole (analgin) can cause anaphylactic shock; it also causes agranulocytosis (with a frequency of 1:500,000) with a fatal outcome. Another unpleasant reaction to this drug is a prolonged collaptoid state with hypothermia (34.5–35.0°), which we observed more than once. All this was the reason for its ban or strict restriction of use in many countries of the world; it is not recommended by WHO in a special letter dated October 18, 1991. Analgin is used only in emergency situations parenterally (50% solution 0.1 ml per year of life) .
It is unacceptable to use nimesulide, an NSAID from the group of COX-2 inhibitors, as an antipyretic in children. Unfortunately, in Russia, the list of indications for its use, along with rheumatoid diseases, pain and inflammatory processes (trauma, dysmenorrhea, etc.), includes the item “fever of various origins (including infectious and inflammatory diseases)” without age restrictions . Of all NSAIDs, nimesulide is the most toxic: according to Swiss researchers [31], a cause-and-effect relationship has been established between taking nimesulide and hepatotoxic effects (jaundice - 90%). In Italy, cases of renal failure have been described in newborns whose mothers took nimesulide. The literature is replete with reports of the toxicity of this drug.
Nimesulide has never been registered in the USA (where it was synthesized), nor in Australia, Canada and most European countries. In Italy and Switzerland, the drug is licensed for adults and is used for strictly defined indications. Spain, Finland and Türkiye, which previously registered nimesulide, have withdrawn their licenses. In those few countries where nimesulide is registered (there are less than 40 of them, the drug is not registered in more than 150 countries), its use is permitted from 12 years of age, only in Brazil it is allowed to be prescribed from 3 years of age.
Sri Lanka and Bangladesh revoked the license for the use of nimesulide in children; in India, a massive campaign to ban this drug in children due to cases of fatal hepatotoxicity ended in victory: the ban was imposed by the country's Supreme Court [32, 33].
Unfortunately, both parents and pediatricians are not yet sufficiently aware of the dangers associated with the use of the “most popular” antipyretics, and therefore the use of analgin, acetylsalicylic acid, and cefekon suppositories in children in our country is not at all uncommon. The “humanitarian action” of manufacturing companies to distribute free nimesulide and the advertising of this strictly prescription drug addressed to parents increase its popularity, although at least one fatal outcome of fulminant hepatitis in a child receiving nimesulide is already known.
The toxicity of paracetamol is mainly associated with an overdose of the drug during the “course” method of its use [34, 35] in daily doses from 120 to 420 mg/kg/day, with more than half of the children receiving drugs in dosages for adults. The indicated single and daily doses of paracetamol are not toxic. The danger of this side effect of paracetamol increases with liver disease, taking hepatic oxidase activators, and in adults, alcohol [36]. With long-term use, cases of nephrotoxicity have been described. Paracetamol taken by pregnant women does not affect the development of the child, while acetylsalicylic acid has a similar effect on the level of attention and IQ of children aged 4 years.
The treatment strategy for a patient with fever involves first of all assessing the likelihood of a bacterial disease. When fever is combined with clear symptoms of the latter, antibiotics are prescribed, and the simultaneous use of antipyretics is less desirable. However, when the above temperature levels are exceeded, muscle pain, headaches, and especially in the presence of convulsions, antipyretics are administered, and it is advisable to prescribe them once, so as not to mask, if possible, the lack of effect of antibiotics, as evidenced by a new increase in temperature after a few hours. But even if a patient with fever has symptoms of only a viral infection, a course of antipyretics is not advisable.
In children with SBI, the main goal of treatment is to prevent the development of SBI, which can be achieved, for example, by administering ceftriaxone (Rocephin, Terzef, Lendacin) (50 mg/kg intramuscularly) [36]. Oral antibiotics reduce the incidence of pneumonia but not meningitis [37]. The point of view according to which antibiotics should be prescribed to all children with SBI is not shared by many authors, believing that in cases where it is possible to monitor the child, antibiotic therapy should be used only in those children who are more likely to develop SBI [38]:
- children 3 months–3 years old with a temperature above 40°, children 0–3 months — above 39°;
- with leukocytosis above 15x109/l and neutrophilia (absolute number of neutrophils above 10x109/l);
- with increased CRP - more than 70 g/l;
- if there are changes in urine analysis or culture;
- if there are changes in the chest x-ray, it should be performed in the presence of shortness of breath (>60 per 1 min in children 0–2 months, >50 in children 3–12 months and >40 in children over 1 year) and/or persistent fever above 3 days;
- upon receipt of positive blood or urine culture data (checking the adequacy of the selected starting antibiotic).
Treatment strategy for febrile seizures
A doctor is rarely present for simple febrile convulsions; doctors usually only catch prolonged or repeated convulsions. For most parents, seizures seem like a disaster, so the doctor’s task is to convince parents of their benign nature.
A child with a generalized attack should be placed on his side, with his head gently pulled back to facilitate breathing; The jaws should not be forcibly opened due to the risk of damaging the teeth; if necessary, the airways should be cleared. If the temperature persists, an antipyretic is administered: paracetamol (Tylenol, Panadol, Prodol, Calpol, Efferalgan UPSA) (15 mg/kg, if it is impossible to administer it orally, a lytic mixture is administered intramuscularly (0.5–1.0 ml of 2.5% solutions of aminazine and diprazine) or metamizole (baralgin M, spazdolzin) (50% solution 0.1 ml per year of life). Rubbing with water at room temperature also helps. For ongoing convulsions, the following is administered sequentially:
- Diazepam (Relanium, Seduxen) 0.5% solution intramuscularly or intravenously at 0.2–0.4 mg/kg per administration (not faster than 2 mg/min) or rectally - 0.5 mg/kg, but not more than 10 mg; or •lorazepam (Merlit, Lorafen) intravenously 0.05 - 0.1 mg/kg (over 2 - 5 minutes); or •midazolam (fulsed, dormicum) 0.2 mg/kg intravenously or as nasal drops.
- For children under 2 years of age, it is recommended to then administer 100 mg of pyridoxine. If convulsions continue after 5 minutes, administer: •a repeat dose of diazepam intravenously or rectally (maximum 0.6 mg/kg over 8 hours); or •phenytoin intravenously (in saline, as it precipitates in glucose solution) at a saturation dose of 20 mg/kg no faster than 25 mg/min.
- If there is no effect, you can administer: •sodium valproate intravenously (apilepsin, depakine) (2 mg/kg immediately, then 6 mg/kg/hour dropwise; dissolved every 400 mg in 500 ml of saline or 5 - 30% glucose solution); or • clonazepam (Clonotril, Rivotril) intravenously (0.25–0.5 mg/kg; this dose can be repeated up to 4 times).
- If these measures are ineffective, sodium hydroxybutyrate (GHB) 20% solution (in 5% glucose solution) 100 mg/kg is administered intravenously or anesthesia is given.
Prophylactic anticonvulsant therapy (diazepam, phenobarbital or valproic acid), although it reduces the risk of recurrent febrile seizures, is not justified and not recommended due to the side effects of these drugs [39]. Single repeated seizures develop in 17%, two repetitions in 9% and three repetitions in 6%; the recurrence rate is higher (50–65%) in children with a first episode before 1 year of age, with a family history of febrile seizures, seizures with low fever, and a short interval between the onset of fever and seizures. 50–75% of recurrent seizures occur within 1 year and all within 2 years [40–45].
Febrile seizures extremely rarely have neurological consequences, including in relation to psychomotor development, academic performance and behavior of children [44, 46]. The developmental prognosis of children who have had febrile seizures, at least at the age of 1–3 years, is, contrary to previously held belief, even better than that of other children due to better memory. In children with simple febrile seizures, the risk of developing epilepsy at age 7 years is only slightly higher (1.1%) than in children without febrile seizures (0.5%), but it increases sharply (9.2%) if developmental disorders are present. a child with complex, especially prolonged seizures and epilepsy in family members [47].
Parent training
It is very important to convey the above data on the rational use of antipyretics to parents. Recommendations for parents can be briefly summarized as follows:
- temperature is a protective reaction, it should be reduced only according to the indications indicated above;
- with regard to antipyretics, it is not “strength” that is important, but safety; to improve the patient’s condition, it is enough to reduce the temperature by 1–1.5°;
- paracetamol is the safest drug, but it is important to strictly adhere to the recommended single and daily dosages;
- paracetamol and other antipyretics should not be prescribed as a “course” in order to prevent a rise in temperature: taking an antipyretic 3-4 times a day is unacceptable due to the risk of preventing the development of a bacterial infection;
- for the same reason, you should not use antipyretics without consulting a doctor for more than 3 days;
- If possible, you should avoid using antipyretic drugs in a child receiving an antibiotic, as this makes it difficult to assess the effectiveness of the latter;
- with the development of malignant hyperthermia with spasm of skin vessels, the administration of an antipyretic drug should be combined with vigorous rubbing of the child’s skin until it turns red; you need to urgently call a doctor.
For questions regarding literature, please contact the editor.
V. K. Tatochenko , Doctor of Medical Sciences, Professor of the Research Institute of Pediatrics of the Scientific Center for Children of Children of the Russian Academy of Medical Sciences, Moscow
Causes
Speaking about how mouse fever is transmitted, it should be noted that the only source of infection is mouse-like rodents. In animals themselves, the infection is asymptomatic, but you can become infected from them, since they release the virus into the environment with excrement, urine, and saliva.
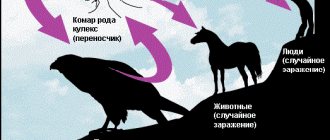
The virus is transmitted aerogenously (airborne dust and airborne droplets), when a person inhales the pathogen in the form of an aerosol. Infection can occur during harvesting, repairs, agricultural work, when spending the night in straw, while working in logging, on farms, etc.
Infection can also occur through breaks in the skin during contact with rodent secretions, an animal bite, or consumption of food and water contaminated with secretions of infected rodents.
The incubation period lasts 7-46 days, but most often its duration is 21-25 days.
Reasons for the spread of HFRS
The source of infection (Europe) is forest mouse-like rodents (bank and red-backed voles), and in the Far East - the Manchurian field mouse.
The natural focus is the distribution area of rodents (in temperate climatic formations, mountain landscapes, low-lying forest-steppe zones, foothill valleys, river valleys).
Routes of infection: airborne dust (inhalation of the virus from dried rodent feces); fecal-oral (eating foods contaminated with rodent excrement); contact (contact of damaged skin with objects of the external environment contaminated with rodent secretions, such as hay, brushwood, straw, feed).
A person has absolute susceptibility to the pathogen. In most cases, autumn-winter seasonality is typical.
Types of morbidity: 1) forest type - they get sick during a short visit to the forest (picking berries, mushrooms, etc.) - the most common option; 2) household type - houses in the forest, near the forest, greater damage to children and the elderly; 3) production path (drilling rigs, oil pipelines, work in the forest); 4) garden type; 5) camp type (rest in pioneer camps, rest homes); 6) agricultural type – characterized by autumn-winter seasonality.
Peculiarities of distribution: • Young people (about 80%) 18-50 years old are most often affected, • More often patients with HFRS are men (up to 90% of cases), • HFRS causes sporadic incidence, but outbreaks can also occur: small 10-20 people , less often – 30-100 people,
After an infection, strong immunity is formed. Repeated diseases do not occur in one person.
Symptoms of mouse fever
The course of murine typhus is divided into several periods, and it is the period that determines how the disease manifests itself. The following periods of the disease are distinguished: initial (febrile), oliguric, polyuric and convalescence.
- In the initial period, the symptoms of mouse fever in adults and children begin to appear acutely. Body temperature rises to 38-40°C, chills , headache, dry mouth, weakness, muscle pain, body aches and other symptoms of intoxication are observed. There may be pain during eye movements and pain in the projection of the kidneys. Around the second day, hemorrhagic enanthema appears on the mucous membrane of the palate. Around the third day, skin hyperemia and a rash in the form of stripes are noted on the face, neck, and chest. During this period, large hemorrhages appear on the skin. There is a possibility of nasal, uterine, and stomach bleeding, which can lead to death.
- During the oliguric period, the symptoms of mouse fever in men and women continue to increase. At this time, the temperature in adults and children continues to remain at 38-40°C for several days. But when it decreases (around day 7), there is no relief. There is pain in the lower back (typical symptoms in men and women during this period), and a severe headache. Hemorrhagic syndrome intensifies. During this period, the patient has dry skin, the face, neck, mucous membranes of the pharynx and conjunctiva are hyperemic. Bouts of repeated vomiting occur that are not associated with food intake, which leads to dehydration. This leads to a decrease in the amount of urine excreted (up to 300-500 ml/day). If the course of the disease is severe, anuria may develop. During this period, the development of oliguria , hyperazotemia , hyposthenuria , and metabolic acidosis . If azotemia (the amount of residual nitrogen) increases, acute renal failure , and uremic coma . At this time, abdominal pain and bloating appear. Signs of mouse fever in men and women from the cardiovascular system are manifested by hypotension , bradycardia , cyanosis . During this period, pulmonary edema may develop, and in severe cases, coma is possible.
- The polyuric period is observed from 9-13 days of illness. At this time, the symptoms of mouse fever in women and men gradually subside. Abdominal and lower back pain become less pronounced, the patient sleeps and eats better. The daily amount of urine increases significantly (up to 3-5 l). At the same time, weakness, dry mouth, and shortness during physical exertion persist. Around day 20, the recovery period begins.
- The period of convalescence - characteristic signs in women and men disappear. of polyuria decreases , body functions are gradually restored. However, the recovery process continues for a very long time - from 3 to 6 months.
Symptoms of mouse fever in children appear the same as in adults. But still, a child’s body can react to the disease individually, so the symptoms in children may differ slightly. Symptoms appear gradually after the child develops a fever. The disease goes through all the stages described above.
How does HFRS develop?
The entry point for infection is the mucous membrane of the respiratory tract and digestive system, where the virus either dies (with good local immunity) or begins to multiply (which corresponds to the incubation period). Then the virus enters the blood (viremia), which manifests itself as an infectious-toxic syndrome in the patient (usually this period corresponds to 4-5 days of illness). Subsequently, it settles on the inner wall of blood vessels (endothelium), disrupting its function, which manifests itself in the patient with hemorrhagic syndrome. The virus is excreted in the urine, therefore the vessels of the kidneys are also affected (inflammation and swelling of the kidney tissue), followed by the development of renal failure (difficulty in excreting urine). It is then that an unfavorable outcome can occur. This period lasts until the 9th day of illness. Then the reverse dynamics occur - resorption of hemorrhages, reduction of renal edema, regulation of urination (up to the 30th day of the disease). Full restoration of health lasts up to 1-3 years.
Tests and diagnostics
The disease is difficult to recognize in the first days. In addition, its symptoms can be confused with the symptoms of other diseases. However, the clinical picture of mouse fever differs from ARVI in the absence of a runny nose and symptoms of respiratory tract damage, and from an intestinal infection - by the later development of symptoms of gastrointestinal damage.
The main diagnostic signs are a sharp decrease in the amount of urine, as well as a deterioration in the person’s general condition after the temperature normalizes. The doctor makes a diagnosis based on the clinical picture, epidemiological history, as well as changes in kidney function characteristic of murine fever.
Laboratory data are taken into account. The following analyzes are carried out:
- general blood test with examination of the leukocyte formula;
- biochemical blood test - determination of creatinine , urea , alanine aminotransferase , aspartate aminotransferase , study of blood electrolytes;
- general urine analysis;
- A coagulation test is performed to assess the severity of the disease.
Instrumental research methods are also practiced:
- Ultrasound of the kidneys;
- X-ray of the lungs;
- fibrogastroduodenoscopy;
- ECG, etc.
Diagnosis of HFRS:
1) If HFRS is suspected, such factors as the presence of the sick in natural foci of infection, the level of morbidity in the population, autumn-winter seasonality and characteristic symptoms of the disease are taken into account. 2) Instrumental examination of the kidneys (ultrasound) - diffuse changes in the parenchyma, pronounced swelling of the parenchyma, venous stagnation of the cortex and medulla. 3) The final diagnosis is made after laboratory detection of IgM and G class antibodies using enzyme-linked immunosorbent assay (ELISA) (with an increase in antibody titer by 4 times or more) - paired sera at the onset of the disease and after 10-14 days.
Treatment with folk remedies
The use of folk remedies for this disease can be an effective auxiliary method. But only if they are pre-approved by a doctor. In addition, one or another method should be used precisely during a certain period of illness, which should also be consulted with a specialist.
- Flax seeds . The decoction is useful for strengthening the kidneys and restoring their function. Prepare a decoction by pouring 1 tsp. seeds with a glass of water. The product must be boiled for 5 minutes. Use half a glass every 2-3 hours for 2 days.
- Birch leaves . To prepare the infusion, pour 100 g of young leaves into 2 tbsp. hot water. After 6 hours, the product should be filtered and drunk 3 times a day, 100 ml.
- Horsetail . 2 tsp. dry raw materials need to be filled with 1 tbsp. boiling water After an hour, strain and drink throughout the day.
- Lingonberry leaves . 2 tbsp. l. raw materials pour 1 tbsp. water and keep in a water bath for half an hour. Drink half a glass 2-3 times a day. You can also prepare an infusion of strawberry leaves, which have a diuretic effect and are a source of vitamin C.
- Dill seeds . Diuretic. 1 tsp. dill should be poured 1 tbsp. water and cook for 5 minutes. Drink 50 ml three times a day.
- Series . Also has a diuretic effect. To prepare the infusion 4 tbsp. l. sequence you need to pour 1 liter of boiling water. After infusing overnight, take 100 ml three times a day.
It is also recommended to prepare decoctions and infusions from herbal collections. To prepare the decoction, 1 tbsp. l. The product needs to be poured into 1 glass of water and boiled for several minutes. Drink half a glass three times a day. Under this scheme, the following fees can be applied:
- 2 parts bearberry and juniper fruit, 1 part licorice root.
- 2 parts each of birch leaves and licorice root, 1 part bearberry.
- 4 parts juniper fruit, 3 parts each angelica root and blue cornflower.
- 5 parts each of knotweed and corn stigmas, 3 parts of hawthorn fruits, 2 parts each of poplar buds, pine and rowan fruits. This remedy should be boiled for 15 minutes, drink three-quarters of a glass an hour before meals, twice a day.
It is also recommended to introduce into the diet some foods that help improve the condition. It is useful to consume pumpkin seeds, berries and currant juice, strawberries, raspberries, blackberries, pumpkin, and figs. Watermelon has a diuretic effect.
During the recovery period, it is recommended to drink vitamin teas. They can be prepared from rose hips, hawthorn, raspberry leaves, strawberries, lingonberries, etc.
It is also recommended to use baths during recovery from illness:
- From horsetail . Add a decoction of 700 g of dry horsetail herb to the bath (boil for 30 minutes before).
- From pine . Boil cones and needles (1-1.5 kg) for half an hour and leave for 12 hours.
Treatment of HFRS
1) Organizational and routine measures • Hospitalization of all patients in a hospital; patients are not infectious to others, therefore they can be treated in infectious, therapeutic, and surgical hospitals. • Transportation without any shocks. • Creation of a gentle protective regime: 1) bed rest - mild form - 1.5-2 weeks, medium-severe - 2-3 weeks, severe - 3-4 weeks. 2) following a diet - table No. 4 without restriction of protein and salt, non-hot, non-rough food, eating small portions often. Liquids in sufficient quantities - mineral water, Borjomi, Essentuki No. 4, mousses. Fruit drinks, fruit juices with water. 3) daily sanitation of the oral cavity - furacillin solution (prevention of complications), daily bowel movements, daily measurement of daily diuresis (every 3 hours the amount of fluid drunk and excreted). 2) Prevention of complications: antibacterial drugs in regular doses (usually penicillin) 3) Infusion therapy: the goal is to detoxify the body and prevent complications. Basic solutions and preparations: concentrated solutions of glucose (20-40%) with insulin for the purpose of energy supply and elimination of excess extracellular K, prednisolone, ascorbic acid, calcium gluconate, Lasix according to indications. If there is no “soaking” effect (that is, an increase in diuresis), dopamine is prescribed in a certain dosage, as well as chimes, trental, aminophylline to normalize microcirculation. 4) Hemodialysis for severe disease, according to certain indications. 5) Symptomatic therapy: - for fever - antipyretics (paracetamol, nurofen, etc.); - for pain syndrome, antispasmodics are prescribed (spazgan, took, baralgin and others); - for nausea and vomiting, cerucal, ceruglan are administered; 7) Specific therapy (antiviral and immunomodulatory effect): virazole, specific immunoglobulin, amixin, iodantipyrine - all drugs are prescribed in the first 3-5 days of illness. Discharge is made upon complete clinical improvement, but not earlier than 3-4 weeks of illness.
Prevention
Preventive measures should be aimed at protecting against rodents and contact with their secretions.
- When in nature, you should avoid dense thickets of grass and store food in places inaccessible to rodents.
- Use masks and respirators when working in rooms with a lot of dust, use gloves.
- Clean rooms where rodents could be present only with a wet method.
- Strictly adhere to the rules of personal hygiene.
- In the house, store food only in places where rodents cannot get into. If the product has been damaged by a rodent, it should not be consumed.
- You should not drink water from open reservoirs.
- Do not handle live or dead rodents without gloves.
- All measures should be taken to prevent rodents from entering apartments and country houses.
- To carry out deratization work, you should contact specialists. It is recommended to regularly carry out deratization in areas of potential rodent habitat.
Today, scientists continue to work on creating a vaccine to prevent HFRS.
Routes of infection
The immune system of a healthy person is easily able to resist the causative agent of hemorrhagic fever. But if the immune system is weakened by any disease, contact with the virus will lead to infection and subsequent development of infection. The main ways the pathogen enters the human body are:
- Air-dust method
. Dried rodent secretions can enter the respiratory system along with inhaled dust. It is not safe to enter long-abandoned premises without a gauze bandage. - Fecal-oral
. Poorly washed vegetables and fruits on which rodents have run can cause infection with the virus. Food supplies must be carefully protected from rats and mice. - Contact
. Contact with contaminated objects. Haystacks and feed warehouses are favorite habitats for rodents.
Outbreaks of infection are rare; usually the disease is isolated, affecting people with the greatest predisposition to the disease. HFRS causes strong immunity that lasts for life.
There are no known cases of recurrent hemorrhagic fever.
Most often, the virus affects the following categories of people:
- Men get hemorrhagic fever much more often than women (up to 90% of recorded cases are infected in males).
- People from 18 to 50 years old who lead an active lifestyle are a group that is at risk (only 20% of cases are children and pensioners)
The pronounced seasonality of the disease (spring-autumn period) is explained by a decrease in the rodent population in winter.
Mouse fever in children
Symptoms of the disease in children manifest themselves in the same way as in adults. However, parents should take into account that the child’s first signs of illness can be confused with signs of other ailments. As a rule, the first signs of the disease are observed 3-10 days after the child has been in contact with the rodent. Sometimes the course may be asymptomatic, and signs will appear only after a few weeks.
Characteristic manifestations of mouse fever in children at different periods of the disease are:
- body temperature up to 40 degrees;
- nausea and vomiting
- pain in muscles and joints;
- visual impairment;
- fatigue, weakness, chills;
- headache;
- severe bleeding from the nose and gums.
To exclude or confirm the disease, it is necessary to consult a doctor at the first warning symptoms.
Diagnosis and treatment of mouse fever in Moscow
Qualified staff of the clinic of JSC "Medicine" in the Central Administrative District of Moscow invites patients with the first signs of the disease for an initial consultation, diagnosis and treatment of mouse fever. All necessary studies and procedures can be completed at the medical center, equipped with advanced equipment from the world's leading manufacturers. Each patient is guaranteed attentive attention, careful development of an individual treatment course, supervision by specialists and confidentiality of personal information. You can make an appointment on the clinic’s website or by calling the indicated telephone numbers in Moscow.
Diet
Diet Table No. 4
- Efficacy: therapeutic effect after 7-10 days
- Time frame: 21 days
- Cost of products: 1120-1150 rubles. in Week
Proper nutrition during illness is an important component of comprehensive treatment. It is necessary to practice fractional meals and consume warm dishes. It is recommended to adhere to diet table No. 4 . But it should be taken into account that the diet differs during different periods of the disease.
- During the period of oligoanuria, protein foods (fish, meat, legumes), as well as vegetables and fruits with a high potassium content, should be excluded from the menu.
- During polyuria, these products, on the contrary, need to be introduced into the diet.
- It is important to control the drinking regime, consuming water taking into account the fluid released.
- After discharge from the hospital, a person should adhere to a gentle, balanced diet for at least six months, consuming healthy foods. You should avoid alcohol, hot and spicy foods.
Prognosis for HFRS
1) recovery, 2) lethal (on average 1-8%), 3) interstitial nephrosclerosis (proliferation of connective tissue in places of hemorrhages), 4) arterial hypertension (30% of patients), 5) chronic pelonephritis (15-20%).
Dispensary observation of recovered patients:
• Upon discharge, a sick leave certificate is issued for 10 days. • Observation for 1 year - once every 3 months - consultation with a nephrologist, blood pressure control, fundus examination, OAM, according to Zemnitsky. • 6 months exemption from physical activity and sports. • Children for one year – medical exemption from vaccinations.
Consequences and complications
Complications and consequences of mouse fever can be very serious. First of all, the consequences of the disease are reflected in the urinary system. Mouse fever can lead to the development of acute renal failure , glomerulonephritis , pyelonephritis , uric acid diathesis , as well as the addition of bacterial infections.
Complications of hemorrhagic fever with renal syndrome may also include the following conditions:
- eclampsia;
- acute vascular insufficiency;
- pulmonary edema;
- kidney rupture;
- pneumonia.
If treated incorrectly and untimely, the development of complications can lead to death.
Complications of HFRS
1) Azotemic uremia . Develops in severe form of HFRS. The reason is the “slagging” of the body due to a serious dysfunction of the kidneys (one of the excretory organs). The patient experiences constant nausea, repeated vomiting that does not bring relief, and hiccups. The patient practically does not urinate, becomes lethargic and gradually develops coma (loss of consciousness). It is difficult to bring a patient out of an azotemic coma, and the outcome is often fatal.
2) Acute cardiovascular failure . Either symptoms of infectious-toxic shock in the initial period of the disease against the background of high fever, or on the 5-7th day of the disease against the background of normal temperature due to hemorrhage in the adrenal glands. The skin becomes pale with a bluish tint, cold to the touch, and the patient becomes restless. The heart rate increases (up to 160 beats per minute), blood pressure rapidly drops (up to 80/50 mmHg, sometimes not determined).
3) Hemorrhagic complications : 1) Tear of the renal capsule with the formation of hemorrhage in the perinephric tissue (in case of improper transportation of a patient with severe lower back pain). The pain becomes intense and persistent. 2) Rupture of the kidney capsule, which can result in severe hemorrhages in the retroperitoneal space. Pain appears suddenly on the side of the rupture, accompanied by nausea, weakness, and sticky sweat. 3) Hemorrhage into the adenohypophysis (pituitary coma). Manifested by drowsiness and loss of consciousness.
4) Bacterial complications (pneumonia, pyelonephritis).
Diagnostics
Diagnosing the disease is extremely difficult , even for an experienced doctor. You need to contact a pediatrician, who will refer you to an infectious disease specialist to confirm the diagnosis.
The main clues are high temperature and contact with rodents, so it is important to give the doctor all possible information.
Further additional studies :
- general urinalysis (increased protein content is observed);
- complete blood count (shows a decrease in platelet levels);
- blood test for antibodies against mouse fever;
- blood biochemistry (determines pathologies in the kidneys);
- coprogram (stool examination);
- PCR (search for viral DNA).
Also, in some cases, the doctor prescribes x-rays, ultrasound and ECG.
Recommendations for the prevention of tick-borne encephalitis in children can be found on our website.
Complications
If the child is not provided with medical care in a timely manner, serious diseases may develop in the future:
- inflammation of the heart muscle (endocarditis);
- infection of the heart valves;
- meningitis;
- pericarditis;
- mumps;
- pulmonary edema;
- sepsis;
- chronic pancreatitis;
- prostate disease in boys.
In the most severe cases, complete kidney failure or cardiac arrest may occur, which can lead to death.
How is it transmitted?
This is an infectious disease of viral origin .
It is transmitted by airborne droplets or direct contact, usually as a result of a mouse bite.
Animal urine and feces can be contagious. Most often, it is inhalation of contaminated air that causes the disease. Infection between people .
The causative agent of the disease is Hantavirus, which has several different strains. Different types of the virus cause 4 main forms of the disease:
- Pulmonary syndrome - affects the lungs of a person. The mortality rate accounts for more than 70% of the total number of cases.
- Cardiac syndrome - the heart muscle is affected. It is extremely rare in Australia and Southeast Asian countries. This form has been little studied.
- Epidemic nephropathy - mainly affects the kidneys. The disease is caused by a strain of Hantavirus called Puumala virus. Found in northern countries, mainly Scandinavian. Mortality rate is low (less than 1%). The disease is mild.
- Hemorrhagic fever affects the kidneys, resulting in kidney failure. Mortality rate is about 10%. Found mainly in Europe. The most common form, which is informally called mouse fever.
How to treat Klebsiella in children? Find out about this from our article.