Reasons for development
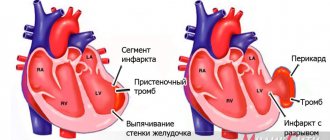
The key cause of the disease, which is called myocardial infarction, is considered to be the formation of a blood clot. Typically, a blood clot forms inside a coronary artery that is already narrowed due to atherosclerosis, a condition in which fatty deposits (or atherosclerotic plaques) accumulate along the inner walls of blood vessels.
Throughout life, fat, calcium, proteins and inflammatory cells accumulate in the arteries, forming atherosclerotic plaques. These deposits are hard on the outside but soft and crumbly on the inside. When the plaque hardens, the outer shell cracks. This is called plaque rupture. Platelets (plates in the blood that help it clot) become trapped in the area, and blood clots form around the plaque. If a blood clot blocks an artery, the heart muscle is starved of oxygen. The muscle cells soon die, causing permanent damage. This is the most common reason, but not the only one.
Slowing of blood flow in the coronary artery can occur when the heart beats very quickly or a person has low blood pressure. If oxygen demand exceeds supply, a heart attack can occur without a blood clot forming. People with atherosclerosis also often suffer from this type of heart attack. Source: Myocardial infarction. Zhmurov D.V., Parfenteva M.A., Semenova Yu.V. Colloquium-journal, 2021. p. 56-61.
In rare cases, coronary artery spasm can also cause a heart attack. During this coronary spasm, your arteries narrow or spasm, cutting off the blood supply to the heart muscle (ischemia). This can happen at rest or under stress, even if the person does not have serious coronary heart disease.
If vascular patency is not restored, there is a risk that recurrent myocardial infarction will develop over time. It will cause even more damage to the heart.
How to distinguish heart disease from others
Many people experience chest pain not necessarily due to any heart disease. Often this occurs due to another illness. If your heart hurts, it can be caused by diseases of the musculoskeletal system, respiratory, digestive and other diseases. However, only a doctor can make an accurate diagnosis after examining the patient.
But any person who has experienced such signs should understand if the heart hurts, what to do and how to recognize that it really is a heart disease. You need to know this in order to promptly consult a specialist in case of some serious pathologies. The signs of the disease may vary; you must learn to recognize them. The most important thing is to distinguish between cardiac and non-cardiac pain. For this purpose, you need to know the duration and intensity of the attack. In addition, it is advisable to have information about other diseases whose symptoms are similar to those of the heart.
The first symptoms of a heart attack
Discomfort in the chest can occur for various reasons. To understand that the heart hurts, it is advisable to know several characteristic symptoms. Seizures are not always accompanied by unpleasant sensations. At the same time, people with other ailments complain that they have difficulty breathing and pain in the left side of their chest. But all this is not a consequence of cardiac diseases.
The earliest signs that indicate that the functioning of the human body’s motor system is impaired most often appear several months, or even years, before the first attack. Therefore, everyone should know how and where the heart hurts. Early signs of the disease that should alert you are:
- Painful sensations behind the ribs. They hit the back, arm, neck, teeth. The left side is most often affected. At the same time, there is shortness of breath, nausea, and increased sweating.
- Discomfort after physical activity, stress, which disappears after rest or nitroglycerin tablets.
- Shortness of breath appears even with moderate exertion, simple work, while eating, and even in a lying position. Before the attack begins, the patient may sleep while sitting or suffer from insomnia.
- Severe fatigue from usual activities can begin long before the first attack.
- Representatives of the stronger sex sometimes develop erectile dysfunction several years before the diagnosis of coronary artery disease.
- Swelling. This symptom is considered the most basic evidence of cardiac dysfunction. At first, the swelling is almost invisible, but becomes larger over time. This is noticeable when a person removes shoes or rings from their fingers. If swelling is observed, you should consult a specialist and undergo an examination.
- Stopping breathing during night sleep, as well as snoring. These signs indicate a predisposition to an attack of heart disease.
Signs of coronary diseases
1. Myocardial infarction
Heart attacks can occur in different ways and how the heart hurts , symptoms in women and men in different situations can be different. In the case of myocardial infarction, everything happens approximately like this:
- There is a feeling of heaviness, pain in the central part of the chest, arm.
- Discomfort spreads to the left arm, neck, throat, and lower jaw.
- You feel dizzy, sweating, your skin becomes paler, and you feel nauseous.
- There is a feeling of heaviness in the stomach, a burning sensation in the chest.
- Anxiety, weakness.
- Rapid pulse.
The course of a heart attack may be different. Sometimes there are no signs at all. Sometimes the patient says that he experiences discomfort in the chest, sometimes there are no such symptoms and the process can be painless. Signs of a major heart attack: shortness of breath, blue lips, etc. very similar to symptoms of acute heart failure.
The duration of such an attack is approximately thirty minutes. Nitroglycerin doesn't help at all.
2. Ischemia
The main manifestation of IHD is angina attacks. In this case, pain occurs in the heart; the symptoms are the same in women and men. Among them:
- cardiopalmus;
- dyspnea;
- cardiac dysfunction;
- inconsistent pulse;
- dizzy, nauseous;
- weakness, sweating.
With coronary artery disease, patients report that they have a burning sensation and pressure in their chest. There is a feeling of being overwhelmed. Often unpleasant sensations are transmitted to the arm, neck, and throat. Most often observed during physical activity, stress and stop when the person remains alone.
With angina at rest, pain in the heart, the causes of which are different, appears at any time, even at night. This form is considered unfavorable.
Inflammatory heart diseases
1. Pericarditis
Pericarditis is an inflammation of the outer lining of the heart, the main symptom of which is a dull pain in the heart area. The pain is usually in the center of the chest, in some cases it radiates to the arm, back, and neck. When swallowing, coughing, etc. discomfort intensifies. Lying down makes it worse, sitting up makes it better. Although the nature of the soreness is usually dull and aching, in some cases it can be acute. Pericarditis is also characterized by rapid heartbeat.
2. Myocarditis
Inflammation of the myocardium is one of the reasons why the heart hurts; approximately 90 percent of people complain about it. Its form can be different, it appears regardless of physical activity, but after some time it can become stronger. Nitroglycerin doesn't help.
Heart valve diseases
If valve disease is present, its severity cannot be judged by symptoms. The patient may not complain about anything and still be in serious condition. Main symptoms:
- Shortness of breath, which is observed not only during high loads, but even during the most usual activities and in a supine position;
- Discomfort in the chest during exercise, breathing in cold air;
- Weakness, dizziness;
- Heart rhythm disturbance. These are, in particular, an uneven pulse, rapid heartbeat, and disturbances in the functioning of the heart.
This pathology often leads to heart failure. Then the following symptoms appear: the legs swell, the stomach bloats, and body weight increases.
Cardiomyopathy
Almost all people who have this pathology complain of pain. As the disease progresses, the way the heart hurts and the symptoms change. At first, the pain is long-lasting, does not depend on physical activity, and nitroglycerin does not help. Feels in different places. Then it is spontaneous or paroxysmal in nature after exercise and most often goes away after taking a nitroglycerin tablet. Its character can be different, its localization is precise, but sometimes it spreads over a large area. Nitroglycerin does not always help.
Arrhythmia
There are several types of arrhythmias. They are characterized by changes in heart rhythm. There are several types of ailments that cause heart pain radiating to the left arm.
Heart defects
These diseases can be acquired or inherited. For a long time they may not talk about themselves. Sometimes your heart hurts; your doctor should tell you what to do. This pain is usually aching, cutting or stabbing in nature. Accompanied by high blood pressure.
Mitral valve prolapse
Aching or pressing pain that appears on the left side is not caused by physical activity. They do not stop after taking nitroglycerin. In addition, dizziness, rapid heartbeat, and headaches may occur in the morning and evening. Possible shortness of breath, lightheadedness.
Aortic stenosis
With this disease, there is a pressing sensation in the chest. There is a strong heartbeat, weakness, fatigue, shortness of breath during physical activity. Over time, shortness of breath and dizziness occur during night sleep. If you suddenly change your body position, you may faint. Attacks of asthma and angina pectoris are possible.
Thromboembolism of the pulmonary artery
This is a very serious condition that requires immediate attention. The first sign of the disease is a stabbing pain in the heart area, which becomes stronger when inhaling and does not radiate to other places. The patient's skin turns blue, blood pressure decreases, shortness of breath and rapid heartbeat appear. Nitroglycerin has no effect.
Aortic pathologies
Sudden, very strong painful bursting sensations in the chest are a consequence of aortic dissection. They are sometimes so painful that a person can lose consciousness. The patient needs emergency medical care.
If there is an aortic aneurysm, there is aching or throbbing pain in the heart, a specialist must decide what to do. If an aneurysm ruptures, the pain becomes unbearable. If measures are not taken, death may occur.
Non-cardiac diseases
1). Intercostal neuralgia. Many people who feel such pain in the heart area mistake it for heart pain. However, in reality they are different. With neuralgia, the pain is sharp and stabbing in nature. They intensify when coughing, deep breathing, sudden turns of the body, etc. This can go away quite quickly, sometimes the pain lasts for several hours. The patient can accurately determine the location of the discomfort; it is located between the right ribs. In the case of angina pectoris, a person experiences a burning, aching feeling that does not go away when the position of the body changes. It is impossible to determine the exact location.
2). Osteochondrosis. This disease is quite easy to mistake for angina pectoris. The person is sure that his heart hurts, the symptoms are as follows: numbness occurs in the left hand, and it becomes more painful when moving. All this is especially similar to angina pectoris when an attack occurs during night sleep. The main difference is that nitroglycerin does not work.
3). Diseases of the central nervous system. In such a situation, patients often complain. However, symptoms vary. This can be regular, short-term, acute or aching pain in the heart area. Neuroses, as a rule, are characterized by a variety of vegetative disorders. A person may experience anxiety, insomnia or, on the contrary, increased sleepiness. Your hands get cold or cold, your head starts to hurt, and much more. Often patients suffering from neuroses complain, talking about numerous symptoms that they do not actually experience. And the “core people” are very reserved in sharing their feelings. Sometimes it is difficult to understand whether a patient has ischemic heart disease or cardioneurosis, since the cardiogram does not show any changes.
4). Disturbances in the functioning of the gastrointestinal tract. However, in this case, heart pain symptoms are somewhat different. They last longer, and the person feels nauseous, vomits, and develops heartburn. The intensity is determined by food intake. Often the symptoms of acute pancreatitis are similar to myocardial infarction. Sometimes exacerbations of gallbladder diseases radiate to the left half of the chest and it seems that the pain is in the heart. To understand what the problem is, you should take antispasmodics. If relief occurs, then the patient has gastrointestinal diseases.
5). Pulmonary diseases. Painful sensations similar to heart pain sometimes appear with pneumonia. This can also happen with pleurisy. But in this case, the pain is acute, intensifying with inhalation and coughing.
What to do?
Every person who feels pain in the chest thinks about what to do next. If there is any suggestion that your heart is hurting, you need to take immediate action. After all, the cause may be serious, in particular myocardial infarction or an attack of angina. Therefore you need to do the following:
- You should calm down and sit down. A stressful state will only worsen the situation.
- You need to try to take a different position. If after this there is relief, there is a possibility that the reason is different. If the pain increases, a pressing pain appears in the heart area, there is a risk that it is angina pectoris.
- It is recommended to allow access to fresh air and open a window.
- To prevent breathing from being constricted, you need to make your clothes looser, unbutton your collar
- If you suspect angina, take a nitroglycerin tablet and place it under your tongue. If relief does not come within a quarter of an hour, you need to take another tablet. You should call for emergency assistance. The medicine does not work for a heart attack.
Finally
Even if the pain in the heart area, the cause of which must be determined by a specialist, has gone away, you need to go to the hospital as soon as possible and get examined. Self-medication is unacceptable.
In Nizhny Novgorod, you can undergo a preventive examination at the Road Clinical Hospital, where professionals work.
Risk factors
Most heart attacks result from atherosclerosis. The risk factors for heart attack and atherosclerosis are essentially the same:
- abnormally high levels of cholesterol in the blood (hypercholesterolemia);
- abnormally low levels of HDL (high-density lipoprotein), commonly called “good cholesterol”;
- high blood pressure (hypertension);
- diabetes;
- family history of coronary heart disease at an early age;
- smoking cigarettes, hookahs, vapes;
- obesity;
- lack of physical activity (too little exercise).
During middle age, the risk of heart attack is higher for men than for women. However, a woman's risk increases when she goes through menopause. This may be the result of a menopause-associated decrease in estrogen, a female sex hormone that may provide some protection against atherosclerosis.
Although most heart attacks are caused by atherosclerosis, there are rarer cases where heart attacks occur as a result of other diseases. These include congenital anomalies of the coronary arteries, hypercoagulability (an abnormally increased tendency to form blood clots), collagen vascular diseases such as rheumatoid arthritis or systemic lupus erythematosus (SLE or lupus), cocaine abuse, coronary artery spasm or embolus (small moving blood clot) , which enters the coronary artery and gets stuck there.
Preventive actions
“First, it is necessary to assess the risk factors when identifying the first signs of metabolic syndrome: increased abdominal circumference, increased blood pressure, increased cholesterol, C-reactive protein, blood sugar. You should immediately contact a cardiologist or endocrinologist. This will allow us to develop an individual plan of preventive measures as early as possible,” says Galina Lazarenko.
It is also worth quitting smoking as early as possible and optimizing physical activity. “All healthy people need moderate-intensity aerobic exercise for 30 minutes a day, 5 times a week, or vigorous-intensity aerobic exercise for at least 20 minutes a day, 3 times a week. Walking 10,000 steps a day every day is required.
Question answer
How can climbing stairs help check your heart health? You can determine the desired intensity of the load by your pulse during training. The maximum heart rate will be equal to the difference between 220 and the patient's age. 60-70% of the obtained value will be the optimal heart rate for moderate-intensity exercise, 75-85% for intense training,” notes the cardiologist.
And, of course, the doctor emphasizes, it is extremely important to normalize nutrition: exclude fast carbohydrates, alcohol, saturated fats (meat with visible fat, for example) from the diet, increase the proportion of foods containing polyunsaturated fats (omega-3 acids - they are contained in sea fish, olive, flaxseed oil), whole grains, vegetables and fruits (at least 5-6 servings per day), reduce salt intake (up to 2-3 grams per day).
Myocardial infarction: symptoms
The nature of the symptoms that develop with each heart attack and the chances of survival are related to the location and extent of the coronary artery blockage.
The first signs of a heart attack include:
- discomfort, pressure, heaviness, tightness, squeezing, or pain in the chest, arm, or under the breastbone;
- discomfort in the back, jaw, throat, or arm;
- stomach fullness, indigestion, or a feeling of choking (may feel like heartburn);
- sweating, upset stomach, vomiting, or dizziness;
- severe weakness, restlessness, fatigue, or shortness of breath;
- fast or uneven heartbeat.
The clinical presentation may vary from person to person or from first to recurrent infarction. Source: Outcomes of Recurrent Myocardial Infarction. Shulaev A.V., Muradimova Z.R., Marapov D.I., Zakirov I.K., Mazitov M.R. Practical medicine, 2021. p. 142-144. Women are more likely to experience symptoms such as upset stomach, shortness of breath, and back or jaw pain. In some heart attacks, patients will not even notice any symptoms (a “silent” myocardial infarction). This is more common in people with diabetes.
Diagnostics
Once a heart attack occurs, the patient needs prompt medical attention to open the blocked artery and reduce the damage. At the first sign of a heart attack, you need to call an ambulance. The best time to treat a heart attack is within 1-2 hours after symptoms appear. A longer wait means more damage to the heart and less chance of maximally complete recovery and rehabilitation after a myocardial infarction. Source: On the issue of overdiagnosis of myocardial infarction. Kim A.O., Kausova G.K. Bulletin of the Kazakh National Medical University, 2021. p. 28-29.
Emergency doctors will ask the person about all the symptoms and perform several tests:
- An ECG (electrocardiogram) can determine how much heart muscle has been damaged and exactly where (types of heart attack). It can also monitor heart rate and rhythm. If there are signs of damage according to the ECG, immediate hospitalization is indicated. The clinic urgently performs additional diagnostic methods.
- Blood tests . Different levels of cardiac enzymes in the blood may indicate damage to the heart muscle. These enzymes are usually found in heart cells. When these cells are damaged, their contents, including enzymes, leak into the bloodstream. By measuring the levels of these enzymes, the doctor can know the size of the heart attack and when it started. The tests can also measure troponin levels. Troponins are proteins inside heart cells that are released when the cells are damaged due to lack of blood supply to the heart.
- Echocardiography . This imaging test can be used during and after a heart attack to see how the heart is working and which areas are most damaged. An ECHO can also determine whether any parts of the heart (valves, septum, etc.) have been damaged due to ischemia.
- Cardiac catheterization . The patient may require cardiac catheterization in the early hours of a heart attack if medications do not relieve ischemia or symptoms. The catheter can provide an image of the blocked artery and help the doctor decide on treatment.
First aid
If you have a heart attack, act immediately. Many people wait too long because they do not recognize warning signs. Take the following steps:
- Call an ambulance. If you suspect a myocardial infarction, do not hesitate to call. Immediately dial 03, 911 or 112. If you do not have access to a telephone, find someone who can take you to the nearest medical facility or heart center. If you drive in this condition, you are putting yourself and others at serious risk.
- Take nitroglycerin if you have been prescribed it. If your doctor prescribed nitroglycerin, take it as directed while you wait for emergency personnel to arrive.
- Take aspirin if it is recommended for you. If you are concerned about your risk of heart attack, ask your cardiologist if you can chew an aspirin tablet. Taking aspirin during a developing heart attack will help reduce damage to the heart by reducing blood clots.
Myocardial infarction: treatment
Upon the arrival of doctors and after taking an ECG, treatment of a heart attack and emergency care depend on how stable the person’s condition is and his immediate risk of death. Doctors have a developed algorithm of actions.
- As soon as possible, the person is given aspirin and often other medications that help prevent unwanted blood clotting in the coronary arteries.
- The person will also be given oxygen to breathe, painkillers (usually narcotic analgesics) for chest pain, beta blockers to reduce the heart's need for oxygen, nitroglycerin to improve blood flow to the heart muscle cells, and statins to lower cholesterol. The patient may be given heparin in addition to aspirin for a stronger anticlotting effect. Emergency hospitalization to a clinic is also important.
- During the initial hospital assessment, the person will be considered for reperfusion therapy, according to clinical guidelines. The goal is to restore blood flow to the damaged heart muscle as quickly as possible to limit permanent damage. Reperfusion is best done mechanically. The patient is taken to the cardiac catheterization laboratory at the hospital. The catheter is passed through a large blood vessel (femoral) to the heart. A dye is injected to detect blockage in the coronary artery.
- The next step is percutaneous transluminal coronary angioplasty (PTCA). In PTCA, another catheter with a small deflated balloon is passed through the blockage and the balloon is inflated to clear the clot and plaque. Most balloon catheters also have a wire mesh, called a stent, on top of the balloon. After the balloon is inflated to clear the blocked artery, the stent is left in place to keep the artery open.
- In addition to aspirin, a second antiplatelet drug is prescribed. The most commonly used drugs are clopidogrel, prasugrel and ticagrelor.
- Reperfusion therapy can also be done with clot-dissolving drugs called thrombolytic agents, such as tissue plasminogen activator (tPA). This drug is used if it takes too long to transfer a patient to a hospital where angioplasty can be performed.
- While in the hospital, the patient begins to undergo the first stages of rehabilitation of patients. He receives daily medications that include aspirin, a beta blocker, an ACE inhibitor (angiotensin converting enzyme) to help the heart work more efficiently, primarily by lowering blood pressure, a statin and a second anti-clotting drug.
Complications of myocardial infarction
Each coronary artery sends blood to a different part of the heart muscle. The extent of muscle damage depends on the size of the area supplied by the blocked artery and the amount of time between the attack and treatment.
The heart muscle begins to repair itself soon after a heart attack. This takes about 8 weeks. As with skin wounds, a scar forms on the damaged area. But new scar tissue moves differently than healthy tissue. Thus, the heart cannot pump as much blood after a heart attack and heart failure is a complication. The extent to which this ability to pump blood is impaired depends on the size and location of the scar.
In addition, some coronary arteries supply blood to areas of the heart that regulate the heartbeat, so a heart attack sometimes causes potentially fatal abnormal heartbeats called cardiac arrhythmiasSource: Complications of Myocardial Infarction in the Elderly. Khalmukhamedov B.T. Eurasian Journal of Cardiology, 2021. p. 29-30.
Prevention
- Check your blood pressure at home. High blood pressure can lead to a heart attack. Sit and rest for 5 minutes before taking your readings. Measure your blood pressure at least 2 times a day at the same time, for example, in the morning and evening.
- Quit smoking. Nicotine and other chemicals in cigarettes and cigars can cause damage to the lungs and heart. Electronic cigarettes or smokeless tobacco also contain nicotine and are no less dangerous.
- Eat a heart-healthy diet. A heart-healthy diet is one that is low in saturated, unhealthy fats and sodium (salt). It helps reduce the risk of heart disease and stroke. Limit the amount of fat you consume to 25-35% of your total daily calories. Your doctor may recommend an eating plan that lowers your cholesterol and blood pressure.
- Limit your sodium (salt) intake. Too much sodium can affect fluid balance. Do the exercises. Ask your doctor about the exercise plan that's best for you. Exercise strengthens the heart, lowers blood pressure and helps prevent heart attacks. The goal is 30 to 60 minutes of activity almost every day.
- Maintain a healthy weight. Ask your doctor how much you should weigh. He can help you create a safe weight loss plan if you are overweight.
- Manage stress. Stress can increase your risk of heart attack. Learn ways to control stress, such as relaxation, deep breathing and music. Talk to someone about what's upsetting youSource: Innovative Methods to Prevent Myocardial Infarction. Volodkin A.A. , Zaikov G.E. NBI-technologies, 2013. p. 103-106.
Sources:
- Myocardial infarction. Zhmurov D.V., Parfenteva M.A., Semenova Yu.V. Colloquium-journal, 2021. p. 56-61
- Outcomes of recurrent myocardial infarction. Shulaev A.V., Muradimova Z.R., Marapov D.I., Zakirov I.K., Mazitov M.R. Practical medicine, 2021. p. 142-144
- Complications of myocardial infarction in the elderly. Khalmukhamedov B.T. Eurasian Journal of Cardiology, 2021. p. 29-30
- On the issue of overdiagnosis of myocardial infarction. Kim A.O., Kausova G.K. Bulletin of the Kazakh National Medical University, 2018. p. 28-29
- Innovative methods for preventing myocardial infarction. Volodkin A.A. , Zaikov G.E. NBI-technologies, 2013. p. 103-106
How to prepare for a doctor's appointment?
- Write down any symptoms you experience, including those that do not seem like symptoms associated with heart disease.
- Write down personal information that includes a family history of vascular or heart disease, stroke, high blood pressure, or diabetes; stressful situations or changes in lifestyle.
- Make a list of all medications, including vitamins and supplements, that you take.
- Ask your family or friends if they remember any information that would indicate heart disease.
- Be prepared to discuss your diet and lifestyle. If you are not following a diet or exercising regularly, be prepared to receive instructions from your doctor about lifestyle changes you should make during treatment.
- Write down questions you want to ask the doctor.
Your appointment time with your doctor is limited, so try to come up with a list of questions that can help you have an effective consultation. Here is a sample list of questions:
- What causes these symptoms and condition?
- What treatment is indicated for me?
- What foods should I eat and what should I avoid?
- What is the acceptable level of physical activity for me?
- How often should I check my cholesterol and have a cardiac screening?
- If I have other health problems, how can I treat them together?
- Are there any restrictions?
- Should I consult other specialists?
- Are there alternative drugs to the drugs that were prescribed to me?
- Are there any brochures or other self-study materials available? What websites do you recommend?