Antiphospholipid syndrome (APS) is an autoimmune process of non-inflammatory origin.
During this process, immune cells produce antibodies aimed at destroying phospholipids - structural formations of vascular and nerve cells, as well as platelet membranes. Of particular danger are complications of antiphospholipid syndrome in pregnant women - stillbirth, premature birth, miscarriages, severe preeclampsia. To prevent this, even at the stage of preparation for pregnancy, the necessary diagnostics must be carried out, acquired or hereditary thrombophilia must be excluded through a blood test.
There are the following types of this pathology:
- catastrophic APS - thrombus formation in various organs in a short period of time (up to seven hours);
- primary – without manifestations of lupus erythematosus or concomitant infectious diseases;
- secondary – against the background of systemic lupus;
- syndrome without specific antibodies;
- APS, manifested by symptoms characteristic of other forms of thrombophilia.
Types of APS caused by the presence or absence of antiphospholipid antibodies:
- seropositive form - in addition to specific antibodies, a lupus anticoagulant was detected in the blood;
- seronegative form – absence of lupus anticoagulant, absence of antibodies to cardiolipin.
Diagnosis of antiphospholipid syndrome and its form is possible only in a modern laboratory equipped with highly sensitive technical equipment and high-quality reagents.
Detailed description of the study
One of the mechanisms of immune defense is normally the production of antibodies - immunoglobulins, Ig - which belong to the gamma globulin fraction of blood serum proteins. By their nature, antibodies are glycoproteins - molecules containing carbohydrate and protein - and are divided into five classes: IgA, IgM, IgG, IgE, IgD. They differ in structure and functions, but have a similar structure. When immunoglobulins react to molecules of the body's own, they are called autoantibodies.
Antiphospholipid syndrome (APS) is an autoimmune disease that includes recurrent thrombosis and obstetric pathology. APS is based on the synthesis of antiphospholipid antibodies and their thrombus-stimulating effect. These immunoglobulins come in several types.
Antiphospholipid syndrome is one of the types of acquired thrombophilias. Thrombophilias are conditions in which thrombosis of blood vessels develops. With APS, blood clots occur both in the venous and arterial beds and can recur (recur) in 70-80% of cases in the same place. Deep vein thrombosis is dangerous due to the high risk of developing embolism - blockage - of the pulmonary vessels.
Thrombocytopenia may also occur with antiphospholipid syndrome. Thrombocytopenia is a condition in which the number of platelets in the blood is less than 150 × 109/L. People with thrombocytopenia have an increased risk of bleeding and bleeding. Numerous small purple spots may appear on the skin, which is why the disease is called thrombocytopenic purpura.
There are primary and secondary APS. The first is diagnosed when the reason causing the increase in antiphospholipid antibodies is unknown. The second is isolated when the underlying disease is known, which causes an increase in the formation of these immunoglobulins and is often associated with chronic stimulation of the immune system. The main four groups of reasons for stimulation are:
- Autoimmune diseases;
- Medications;
- Infectious diseases: viral and bacterial, the production of antiphospholipid antibodies is especially common in HIV infection and syphilis;
- Malignant tumors.
A number of drugs increase the concentration of antiphospholipid antibodies, including phenothiazines and other drugs that cause drug-induced lupus: chlorpromazine, hydralazine, phenytoin, procainamide and quiniline.
Antiphospholipid antibodies increase in both viral and bacterial infections. However, with them the increase is transient - short-term - and their appearance should be distinguished from APS.
Obstetric pathology in APS is associated with miscarriage. Miscarriage caused by an increased concentration of antiphospholipid antibodies is possible at any stage, but more often occurs in the second or third trimester. Fetal death is a consequence of thrombus formation in the small vessels of the placenta, due to which the latter ceases to perform its functions and further pregnancy becomes impossible.
A comprehensive study for APS includes the following groups of antiphospholipid antibodies:
AT to cardiolipin.
Cardiolipin is a phospholipid that is part of biological membranes, namely, it is found in the mitochondrial membrane, one of the cell structures where it participates in metabolic processes. In antiphospholipid syndrome, immunoglobulins are produced in response to cardiolipin, so their determination with the appointment of the appropriate analysis is one of the main points in the correct diagnosis.
AT to phospholipids.
These autoantibodies are aimed at damaging the main components of the biological membranes of human cells. These components are phospholipids. Of these molecules, the most antibodies are produced to phosphatidylserine, which is located on the inner surface of platelets and on the membranes of the cells of the inner layer of blood vessels (endothelium). Phosphatidylserine takes an active part in the formation of a blood clot (thrombus), and when antibodies to this molecule are produced, inadequate thrombus formation occurs.
Lupus anticoagulant (LA).
VA is a group of antibodies to phospholipids, which also increase the risk of blood clots. It was first isolated from patients with systemic lupus erythematosus, but is currently included in one of the criteria for defining antiphospholipid syndrome.
Antibodies to beta-2 glycoprotein.
These ATs are one of the main markers of APS. Their identification in cases of suspected APS is recommended by Russian and foreign clinical guidelines. Beta-2 glycoprotein immunoglobulins are often associated with secondary antiphospholipid syndrome secondary to systemic lupus erythematosus.
Antibodies to prothrombin.
Prothrombin is a protein involved in blood clotting processes. Antibodies to it directly contribute to the development of APS symptoms.
This analysis can determine the presence of APS with a high degree of probability, is widely used in clinical practice, is affordable and has no absolute medical contraindications. Venous blood must be donated for testing.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
Signs and symptoms of antiphospholipid syndrome
The clinical signs of all forms of APS are caused by thrombosis. Symptoms of antiphospholipid syndrome depend on the localization of the process, the size and type of vessel, and the rate of development of thrombosis. When small vessels are affected, the symptoms of antiphospholipid syndrome develop slowly, gradually progress, and resemble organ damage by a chronic inflammatory process. When large vessels are damaged, the function of the corresponding organ is dramatically disrupted, which leads to catastrophic changes.
Manifestations of damage to certain organs and systems:
- lower extremities: swelling, soreness, hyperemia, ulceration, gangrene;
- nervous system: encephalopathy, migraine, hearing loss, neuropathy, paresthesia, amnesia and microstroke;
- heart: cardiomyopathy, hypertension and heart attack;
- kidneys: signs of renal failure;
- liver: symptoms of portal hypertension;
- skin: bluish mesh, rash and gangrene of the fingers;
- pregnancy: placental abruption and spontaneous abortion.
Rarely the vessels of the lungs, stomach or intestines are affected.
When the lower extremities are affected, patients complain of intense pain in the legs, which intensifies after physical activity and decreases after rest. Some patients note increased pain when the limbs drop below the level of the head. The skin of the legs is pale, sometimes bluish, cold to the touch, and with a chronic, slowly developing process, trophic changes are noticeable.
When the central nervous system is damaged, patients complain of attacks of headaches. The pain is most often localized in the right or left half of the head, intense, aggravated by the slightest noise or even light. Sometimes attacks are preceded by auditory or visual hallucinations, flashes of light before the eyes.
The development of encephalopathy is indicated by forgetfulness, inability to orientate oneself in place and time, dizziness, and decreased cognitive abilities. Intellectual tasks that the patient previously handled without problems become overwhelming. Sensitivity in the limbs or certain parts of the body decreases, a tingling sensation appears, and tolerance to low temperatures worsens. When the cardiovascular system is damaged, high blood pressure and periodic pain in the heart are noted. Despite adequate therapy, the patient experiences cardiovascular disasters - strokes and heart attacks.
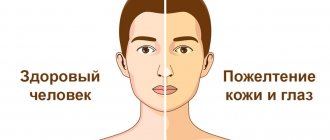
Kidney failure develops gradually. At the initial stages, patients feel satisfactory. With significant dysfunction, nausea, vomiting, general weakness, dizziness appear, and the amount of urine decreases. The level of creatinine and urea in the blood increases significantly - the main indicators of nitrogen metabolism, which are normally excreted by the kidneys. Liver damage is indicated by the accumulation of fluid in the abdomen, a feeling of heaviness and pain in the right hypochondrium, and bitterness in the mouth. Jaundice may develop.
Pregnant women are a special category of patients with APS. It is almost impossible for such patients to carry and give birth to a healthy child without adequate accompanying therapy. In most cases, women are diagnosed with frozen pregnancy in the early stages and spontaneous miscarriages. Even if the pregnancy is not terminated early, the likelihood of premature birth, intrauterine fetal death and premature placental abruption is very high.
References
- Guyton, A.K., Hall, J. Medical physiology / ed. IN AND. Kobrina. - M.: Logosphere, 2008. - 1296 p.
- Internal diseases in 2 volumes: textbook / ed. ON THE. Mukhina, V.S. Moiseeva, A.I. Martynova, 2010. - 1264 p.
- Secrets of rheumatology. - St. Petersburg: BINOM Publishing House, 1999. - 768 p.
- Reshetnyak, T.M. Antiphospholipid syndrome: diagnosis and clinical manifestations (lecture). Scientific and practical rheumatology, 2014. - No. 1.
- Federal clinical guidelines. Laboratory diagnosis of rheumatic diseases, 2014. - 12 p.
- Makarenko, E.V. Antiphospholipid syndrome. Problems of health and ecology, 2021. - No. 4 (54).
- Miyakis, S., Lockshin, M., Atsumi, T. et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J ThrombHaemost, 2006. - Vol. 4(2). - P. 295-306.
APS during pregnancy
To prevent the development of dangerous complications, the doctor prescribes treatment from the very beginning of pregnancy.
If there are appropriate indications, the specialist may prescribe anticoagulants (drugs that reduce blood viscosity) and antiplatelet agents (substances that prevent red blood cells and platelets from sticking together).
Additionally, it is recommended to take B vitamins (including folic acid) and magnesium.
If a pregnant woman suffers from APS, she develops progesterone deficiency, so from the very beginning of pregnancy the doctor prescribes progesterone drugs.
Pregnancy management should be carried out under the supervision of an experienced hemostasiologist. Careful monitoring of the condition of the expectant mother and baby is necessary, as well as adjustment of the dosage of drugs based on research results. In the absence of adequate treatment, the likelihood of a successful pregnancy outcome is very low. If therapy is started in a timely manner, the chances increase markedly.
Antiphospholipid antibodies in the blood - normal or pathological?
Sometimes the level of antiphospholipid antibodies can be elevated in a healthy person. In 12% of people, these antibodies are present in the blood, but they do not develop the disease. The older the person, the higher the levels of pathological immunoglobulins may be. There is also a possibility of a false-positive Wasserman reaction, for which the patient should be prepared. The main thing is not to panic and undergo a comprehensive diagnosis.
Video: APS and other thrombophilias in obstetrics:
Author of the article:
Volkov Dmitry Sergeevich |
Ph.D. surgeon, phlebologist Education: Moscow State Medical and Dental University (1996). In 2003, he received a diploma from the educational and scientific medical center for the administration of the President of the Russian Federation. Our authors
Treatment
After a thorough clinical examination, interpretation of laboratory data and medical history, a rheumatologist at the Yauza Clinical Hospital develops an individual treatment regimen for APS for each patient. Its components may be:
- indirect anticoagulants and antiplatelet agents;
- glucocorticoids;
- immunosuppressants;
- aminocholines;
- selective NSAIDs;
- immunoglobulins;
- complexes of vitamins and microelements.
Extracorporeal hemocorrection in the treatment of antiphospholipid syndrome
To reduce the amount of autoantibodies in the patient’s blood, increase the body’s sensitivity to drug therapy, and reduce the likelihood of developing side effects of drugs, our specialists use an innovative method for treating APS - extracorporeal hemocorrection. The following EG methods are used:
- cryoapheresis;
- cascade plasma filtration;
- immunosorption;
- high-volume plasma exchange;
- extracorporeal pharmacotherapy;
- photopheresis
The use of extracorporeal technologies in the treatment of APS helps to stop the autoimmune process, alleviate the course of the disease, as well as the onset of pregnancy and its favorable gestation in almost 90% of cases.
In addition, the course of hemocorrection in 100% of cases normalizes blood clotting ability, which eliminates the increased risk of thrombosis and thromboembolism characteristic of APS.
Why us?
- Ultra-modern equipment. The qualifications of our specialists, expert equipment and modern techniques allow us to timely and accurately diagnose APS.
- Consultation of related specialists. The patient is examined by a council of doctors, this especially applies to pregnant women.
- Comfortable conditions. Our rheumatologists devote maximum time to each client. All services are provided in one building in the center of Moscow, which saves effort and time.
- Innovation. The use of high-tech treatment methods ensures the success of therapy.
Use the full potential of modern medicine to maintain your own health and give life to your child - contact a rheumatologist at the Yauza Clinical Hospital.
You can see prices for services