A hiatal hernia (HH, hiatal hernia, gastric hernia) is an enlargement of the esophageal opening of the diaphragm through which the esophagus normally penetrates into the abdominal cavity, and with a hernia, an abdominal organ, most often the stomach, penetrates into the chest. Sometimes intestinal loops and, extremely rarely, the spleen penetrate into the chest with hiatal hernia. This disease is quite common, it is found on average in 40% of the world's population. Fortunately, for the majority it does not cause any problems, but in 5 - 7% of all gastroenterological patients, complaints are caused by this particular disease (Figure 1).
Causes of hiatal hernia
Most often, it is not possible to find out the cause of the development of this disease in a particular patient. In general, hiatal hernia is a multifactorial disease and it can be difficult to identify one single cause unless there is a clear connection with trauma.
The following reasons for the development of a hiatal hernia are identified:
- Increased intra-abdominal pressure, for example due to overeating at night, or chronic constipation. Another reason for increased intra-abdominal pressure, and hence the development of hiatal hernia, is heavy physical labor.
- Congenital degenerative changes in the ligamentous apparatus and connective tissue.
- Age and associated connective tissue degeneration. Therefore, in these patients it is not uncommon to have a combination with an inguinal or ventral hernia.
- Blunt abdominal trauma.
- The presence of chronic diseases that disrupt the normal motility of the gastrointestinal tract (peptic ulcer, reflux esophagitis, cholelithiasis, diseases of the large intestine).
- Excess weight. In overweight people, intra-abdominal pressure increases, which leads to “squeezing” the stomach into the chest
Etiology
Symptoms of a hiatal hernia are quite specific
The diaphragm is an organ that acts as a partition separating the abdominal and thoracic cavities. It consists of two types of tissue: muscle and connective.
The esophagus passes through a hole in the diaphragm, surrounded by bundles of muscles. Displacement of organs occurs due to weakening of the ligamentous apparatus of the diaphragm, since in a number of age-related changes the tissues undergo degenerative processes, lose elasticity and, in severe cases, atrophy. As a result, a hernia forms.
In children, the development of the disease occurs in the embryonic phase. This type of pathology is called congenital. The formation of a hernia in the esophagus can often provoke increased intra-abdominal pressure resulting from:
- Frequent constipation
- Hard work
- Injuries
- Severe obesity
- Ascites
- flatulence
Often, a hiatal hernia is a concomitant disease of other abdominal organs:
- Duodenal ulcers
- Pancreatitis
- Cholecystitis
- Gastroduodenitis
The disease can develop as a result of shortening of the esophagus, which is observed with scar-inflammatory deformation resulting from:
- Reflux esophageal disease
- burn
- Ulcers
The prevalence of the disease competes with pancreatitis and gastritis. Elderly and frail people are more often susceptible to it.
Classification of hiatal hernia
In our country, unfortunately, there are many classifications of this disease, but the most common classification proposed by B.V. Petrovsky and N.N. Kanshin. Following it, the following variants of the hiatal hernia are distinguished:
Axial:
- fixed
- unfixed
Without shortening of the esophagus
- cardiac
- cardiofundic
- subtotal
- total
With shortening of the esophagus
1st degree of cardia is fixed 4 cm above the diaphragm
Grade 2 cardia is fixed more than 4 cm in the chest
Paraesophageal
- fundamental
- antral
- intestinal
Now let's figure out what is what. So, a hiatal hernia is called axial if the esophagogastric junction is located above the diaphragm. It is called cardiac if only the cardia (upper part of the stomach) is located above the diaphragm, cardiofundal hernia is called if both the cardia and the fundus of the stomach go into the mediastinum, subtotal hernia is called if 2⁄3 of the stomach goes into the mediastinum (above the esophageal opening of the diaphragm), and, accordingly, total This is when the entire stomach is located in the chest.
A paraesophageal hernia is a situation when the esophageal-gastric junction (cardia of the stomach or simply cardia) is located in the abdominal cavity, and any part of the stomach or other organ penetrates through the esophageal opening of the diaphragm into the mediastinum (Figure 2).
Complications
The most common complication and manifestation of sliding hiatal hernias is reflux esophagitis, which is caused by upward reflux of gastric contents. In addition, the patient may develop:
- peptic ulcer of the esophagus;
- cicatricial changes (strictures) with narrowing of the esophagus;
- bleeding from the veins of the hernial part;
- shortening of the esophagus;
- Barrett's esophagus (replacement of the multilayered epithelial covering of flat forms of esophageal epithelium with single-layer cylindrical cells from the stomach or intestines), a precancerous disease.
Complaints with esophageal hernia
The most common complaint with hiatal hernia is heartburn.
. You can read more about heartburn here. Heartburn most often occurs at night or after eating while lying down; it often occurs after physical activity, especially in an inclined position. Sometimes heartburn is accompanied by chest pain. Most often, relief from this condition comes from taking antacids, such as reni, or drugs that reduce the production of hydrochloric acid in the stomach, such as omeprazole.
The next common symptom of this disease is pain
. It is of a burning nature, localized behind the sternum, and radiates to the right shoulder. The pain intensifies most often after eating or lying down. Sometimes it is accompanied by heart rhythm disturbances. Most often, the pain goes away after belching, or if the patient gets up and walks around. Sometimes pain in people with a hiatal hernia is confused with pain in the heart, especially since with hiatal hernia pain is often accompanied by arrhythmia. Pain is most often relieved by antispasmodics, no-spa, etc.
Another complaint among patients is belching
. Belching occurs with both food debris and air. Sometimes it is uncontrollable and occurs without reference to food intake. Often, this lack of control and unpredictability of the occurrence of the latter is the main reason for surgical treatment of patients with hiatal hernia.
Regurgitation
- throwing food into the oral cavity while lying down or bending over. This complaint is relatively uncommon and occurs more often with large hernias.
Dysphagia
- difficulty passing food through the esophagus, develops at the stage of complications of the hiatal hernia. Dysphagia is caused either by an inflammatory process in the walls of the esophagus, or by a cicatricial stricture (narrowing) of the esophagus. Dysphagia requires hospital treatment
Extraesophageal manifestations of hiatal hernia are also distinguished. The most common of this group of complaints is cough.
. Often a cough accompanies the patient for years. It occurs more often in a lying position or when bending over, after eating. The cough is accompanied by a constant sore throat.
The second most common extraesophageal complaint is arrhythmia
. Most often, arrhythmia occurs with a large hiatal hernia, when most of the stomach is in the chest. In this case, the arrhythmia is associated with eating or bending, or occurs in a lying position. Typically, when examining such patients, cardiologists do not find heart pathology. Another manifestation of hiatal hernia is chronic diseases of the ENT organs, pharyngitis and laryngitis. The connection between laryngitis or pharyngitis and the hiatal hernia can be confirmed or refuted using daily pH measurements of the esophagus.
In addition, the consequence of a hiatal hernia can be dental damage, hoarseness, bronchitis, and bronchial asthma.
Clinical symptoms
Half of the cases are characterized by the absence of symptoms or mild clinical manifestations. This applies to small-sized hiatal hernias. The larger the hernial protrusion, the more pronounced the symptoms are observed.
The disease is characterized by pain, but its localization may vary. In addition to the epigastric region (the “solar plexus” area), pain sensations can be concentrated behind the sternum with irradiation to the back and between the shoulder blades (simulating a heart attack) or mask the disease as pancreatitis (have a shingles nature).
What signs of pain indicate the presence of a hiatal hernia?
- The appearance of pain after eating, lifting heavy objects, with bloating and taking a horizontal position of the body, when bending the body forward.
- Improvement after vomiting, belching, drinking water or taking an upright body position.
Symptoms accompanying severe pain when a hernia is strangulated:
- nausea;
- increased respiratory rate;
- vomiting streaked with blood;
- increased heart rate;
- cyanosis of the skin and mucous membranes;
- lowering blood pressure.
Sometimes the hiatal hernia causes cardiac arrhythmias. This must be taken into account during long-term and unsuccessful treatment with a cardiologist.
Gastroesophageal reflux disease (GERD) is considered a frequent companion of hiatal hernia, which provokes the appearance of a new symptom complex resulting from digestive disorders:
- vomiting air, eaten food or bile.
- Regurgitation not preceded by nausea. The symptom occurs when the body is positioned horizontally at night, following a heavy dinner, and can lead to the development of complications in the form of diseases of the bronchopulmonary system.
Other clinical manifestations characteristic of hiatus hernia:
- Dysphagia is a specific symptom characterized by impaired movement of food through the esophagus after swallowing. This complaint is provoked by drinking hot or cold water, swallowing a poorly chewed food bolus or large amounts of liquid, as well as stress factors.
- Severe heartburn.
- Persistent hiccups.
- Burning sensation in tongue.
- Hoarse voice.
Course of hiatal hernia
HH is a very common disease. As I already wrote, up to 40% of the world's population have this disease, but most of them do not even suspect it. Problems begin when the sphincter between the esophagus and stomach stops working and the contents of the latter enter the esophagus. Or if the hernia of the PAD reaches a large size and causes complications associated with neighboring organs (arrhythmias, pneumonia, etc.). In most cases, with proper treatment, the course of the disease is favorable, and conservative therapy is sufficient. Therapy is aimed at reducing the reflux of gastric contents into the esophagus, relieving inflammation, and normalizing gastrointestinal motility. If conservative therapy is not effective, surgical intervention must be resorted to.
Traditional methods of treatment
It is worth learning from traditional medicine how to treat a hernia only as an additional method of improving well-being, if the doctor who determined the tactics of treatment with diet and medication approves the auxiliary intervention.
A good addition to your diet would be to use mild, anti-inflammatory chamomile or lightly brewed green tea. When choosing infusions and herbs, you should look for an option that will reduce stomach acidity, heartburn and abdominal discomfort. Often recommended ginger and lemon teas for hernia and other gastroenterological diseases are contraindicated.
Complications of hiatal hernia
Erosion and ulcers of the esophagus occur in 7 - 9% of cases in patients with hiatal hernia. This complication is associated with the aggressive action of gastric juice, which enters the esophageal mucosa. Usually the presence of ulcers and erosions is accompanied by the most severe complaints of patients. The danger of an ulcer is that if not treated correctly, a scar may form at the site of the ulcer, which in turn can lead to obstruction of the esophagus. In the presence of multiple erosions, chronic anemia may develop. The presence of an ulcer in the esophagus is an indication for surgery.
Bleeding and anemia with hiatal hernia occur in 11 - 20% of cases. Bleeding most often occurs due to vomiting, for example after poisoning. Such bleeding can be quite massive and require emergency hospitalization. Bleeding can be manifested by vomiting blood, or so-called coffee grounds, dark coffee-colored contents. Sometimes bleeding may appear as black, tarry stool. In case of repeated episodes of bleeding, surgical treatment is indicated.
Anemia occurs in two cases. The first is chronic minor blood loss against the background of the presence of multiple erosions of the esophageal mucosa. This bleeding occurs periodically and goes unnoticed, and can continue for months. The second reason is a violation of iron absorption against the background of inflammatory changes in the stomach. This anemia is called iron deficiency and develops when most of the stomach is in the chest. Anemia manifests itself as severe weakness.
Cicatricial stricture of the esophagus. With a long-term inflammatory process in the wall of the esophagus against the background of the hiatal hernia, scars are formed that narrow the lumen of the esophagus. A stricture appears, a disruption in the passage of food through the esophagus. This complication is manifested not by the ability to eat, first with solid food, but as the process progresses, with liquid
Incarcerated hiatal hernia. A very rare complication, but extremely dangerous, which in the absence of qualified medical care leads to death. This complication is manifested by the sudden appearance of severe bursting pain in the chest, a feeling of fullness. Patients constantly try to induce belching, which is either impossible or does not bring relief. This complication requires emergency surgery.
To summarize, I would like to repeat that with proper treatment, complications of the hiatal hernia develop quite rarely.
Gymnastics
For hiatal hernia, physical therapy is recommended. The following exercises help a lot:
- Lie on your side and rest your head on the cushion. Inhale deeply and inflate your stomach as much as possible, then exhale slowly and relax. Repeat 4-5 times.
- Get on your knees, straighten your back, inhale and slowly bend to the right, exhale and return to the starting position, repeat the exercise 6-7 times.
- Lie on your back. Breathing is even and calm. Slowly turn to your left and then to your right side, trying not to lose your breath.
Diagnosis of hiatal hernia
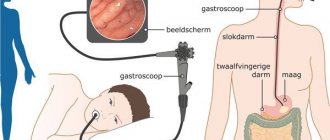
The main role in diagnosis is played by X-ray examination with barium and gastroscopy.
X-rays are performed on an empty stomach using a barium contrast solution. The doctor monitors the passage of contrast through the esophagus and stomach on the X-ray machine screen. Thanks to X-ray examination, it is possible to identify the size of the hernia, the presence or absence of reflux of gastric contents into the esophagus, the presence or absence of disturbances in the passage of contrast through the esophagus and stomach.
Gastroscopy allows you to assess the condition of the esophageal mucosa, the presence or absence of inflammation, erosions, ulcers, and the presence of narrowing. In the vast majority of cases, these two studies are sufficient to make the correct diagnosis. In some cases, a CT scan is performed to evaluate the presence or absence of a hiatal hernia and its size. If there are non-esophageal manifestations or an unclear clinical picture, daily pH measurements are performed. A thin probe is installed into the lumen of the esophagus for 24 hours, which records the reflux of gastric contents into the esophagus, making it possible to identify the connection between complaints and reflux of gastric contents.
Diagnostics
The main signs of the disease are determined by x-ray examination. To identify an abnormal location of the end of the esophagus and stomach, use:
- general visual X-ray examination with contrast of the initial digestive organs - currently rarely used;
- X-ray (series of images) of the esophagus and stomach.
The patient is photographed in the following position:
- lying down,
- standing,
- on the side
- in the knee-elbow Trendelenburg position.
Radiologists take into account, as a direct sign, a clear displacement of part of the stomach into the chest cavity. Indirect ones include:
- disturbed shape of the gas bubble or its absence, change in size;
- increase in the angle of His;
- signs of reflux reflux;
- movements of the esophagus that are the opposite of proper peristalsis.
Ultrasound diagnostic specialists consider it possible to participate in the examination; the picture differs from the radiological signs (right)
Esophagogastroscopy shows:
- non-closing walls of the esophagus in the diaphragmatic area (picture of “gaping of the cardia”);
- the cardiac section is located higher than usual due to shortening of the esophagus;
- gastroesophageal reflux;
- foci of proliferation of foreign epithelium.
Endoscopy helps to identify the severity of reflux influence and possible transition to a neoplasm.
Additional methods include:
- esophagomanometry,
- scintigraphy,
- intraesophageal pH-metry.
Conducting a general clinical examination helps to identify complications:
- stool analysis can detect early signs of bleeding;
- blood test shows anemia, infection;
- An ECG is absolutely necessary to exclude atypical angina.
Differential diagnosis is always carried out:
- with different types of diaphragmatic hernias;
- cicatricial changes in the esophagus;
- peptic ulcer;
- malignant neoplasm;
- disorders associated with increased pressure in the portal vein;
- angina pectoris;
- gallstone disease.
Treatment of hiatal hernia
In the vast majority of cases, conservative therapy is carried out, which in fact is symptomatic and is aimed at improving the well-being of patients and preventing the development of complications. The main cause of complaints from patients is the reflux of aggressive gastric contents into the esophagus. Therefore, proton pump inhibitors (esomeprazole, Nexium, etc.) are prescribed. This is a group of drugs that reduce the acidity of gastric juice, thereby minimizing the damaging effect on the esophageal mucosa. Enveloping drugs in the form of suspensions are also used, such as Gaviscon, Maolox, Almagel. These drugs effectively reduce the acidity of gastric juice and, by enveloping the walls of the esophagus, protect them from reflux. And the third group of drugs are prokinetics (Motilium, Ganaton). These are medications that improve and normalize the motility of the esophagus and stomach, thereby reducing the frequency of reflux.
This therapy leads to improved well-being and quality of life. Unfortunately, up to 80% of patients experience a relapse of complaints immediately after stopping taking the drugs and therefore have to take them constantly. Complete removal of a hiatal hernia is only possible through surgery. You can read about surgical treatment of hiatal hernia here
Author: Ph.D. Siyukhov R.Sh.
Treatment methods for sliding hiatal hernia
After confirmation of the diagnosis, treatment should begin immediately: the sooner it is prescribed and performed, the lower the risk of complications and the lower the risk of surgical intervention.
An uncomplicated sliding hernia is treated conservatively by prescribing a set of three measures:
Diet
The mandatory and main method of treating a sliding hiatal hernia is constant adherence to a diet.
Patients are recommended to eat split meals (frequently, every 3–4 hours, in small portions of 200–300 g) with the exception of fried, fatty, spicy, salty foods, pickled, smoked and other foods that irritate the mucous membranes and stimulate the secretion of gastric juice.
The basis of the diet consists of boiled, stewed and steamed dishes from vegetables, cereals, milk, lean meat, and fresh fruits.
With true dysphagia, food should have a ground, semi-liquid consistency. You should eat no later than 1 hour before bedtime, and after eating it is advisable to rest for 15–30 minutes in a sitting or reclining position (but not lying down!).
Normalization of lifestyle
A complete cessation of smoking, alcohol, sufficient rest, and dosed physical activity are required. Physical exercises that can increase pressure in the abdominal cavity (with stress on the abs, flexion) are prohibited.
Postoperative period
In cases of uncomplicated course of the disease and successful laparoscopic surgery, postoperative management of patients does not go beyond standard measures (pain relief according to indications, antibiotic prophylaxis during surgery and on the 1st day after it, nutrition with liquid food from the 1st day, removal of safety drainage through 12-24 hours). The duration of hospitalization is on average from 2 to 5 days.
If complications develop, appropriate therapy is provided. To evaluate the results of treatment, it is recommended after 3-6 months. perform gastric X-ray, endoscopy and pH monitoring.