- home
- general surgery
- Esophageal diverticula
To identify a diverticulum of the esophagus, its localization, as well as choose the correct surgical treatment tactics, you must send me a complete description of gastroscopy, X-ray of the esophagus and stomach with barium, preferably an ultrasound of the abdominal organs, by indicating your age and main complaints. Then I will be able to give a more accurate answer to your situation.
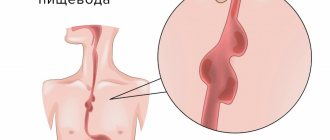
Esophageal diverticulum
- this is a protrusion of the submucosal layer and mucous membrane of the esophageal wall through a defect in its muscular lining.
The first description of esophageal diverticula was made by the English anatomist Ludlow (1764). Our Russian scientist Rokitansky (1840) divided all esophageal diverticula into pulsion and traction and described epibronchial diverticula. The German scientist Zenker (1877) characterized esophagopharyngeal diverticula.
Diverticula can be congenital or acquired (they are much more common), the latter arise as a result of inflammatory changes in the wall of the organ and surrounding tissues.
Fig. 1 Location of esophageal diverticula (1- left main bronchus, 2- peribronchial diverticulum, 3- trachea, 4- lower pharyngeal constrictor, 5- Zenker diverticulum, 6- right main bronchus, 7- esophagus, 8- epiphrenic diverticulum, 9- diaphragm, 10- abdominal part of the esophagus).
In their origin, they can be pulsational (based on an increase in pressure in the lumen of the organ with subsequent protrusion of the submucosal layer and mucous membrane) and traction (the inflammatory process around the esophagus pulls its wall towards itself with the formation of a protrusion).
Depending on the location, diverticula of the esophagus are divided into (Fig. 1): - pharyngoesophageal (the so-called Zenker diverticula), - epibronchial (located in the middle section of the esophagus, in the bifurcation area - the most common localization) - epiphrenal (located above the diaphragm).
Diverticula are observed more often after 50 years, mainly in men.
Pharyngeal-esophageal (Zenker's) diverticulum.
The main role in the pathogenesis of the formation of this type of diverticula is achalasia (inability to relax) of the cricopharyngeal muscles, which results in a violation of the opening of the upper esophageal sphincter in response to swallowing. Excessive intraluminal pressure pushes the submucosal layer into the resulting muscle defect. The diverticulum then descends between the posterior wall of the esophagus and the spine. The inner surface of the diverticulum is covered with a mucous membrane; it may have superficial erosions, foci of inflammation and scars.
Classification
Squamous cell carcinoma of the esophagus, like all malignant tumors, is classified and staged in accordance with the international TNM classification (8th revision).
TNM Esophageal Cancer Staging System (UICC, 8th edition)
Primary tumor
Tx The primary tumor cannot be assessed;
T0 No evidence of a primary tumor;
Tis Carcinoma in situ/high grade dysplasia;
T1 Tumor growth into the lamina propria or submucosal layer;
T1a Tumor involves the lamina propria or lamina muscularis mucosa T1b Tumor invades the submucosal layer;
T2 Germination of the muscle layer;
T3 Germination of adventitia;
T4 Germination of adjacent structures;
T4a Pleura, peritoneum, pericardium, diaphragm, vein of azygos;
T4b Adjacent anatomical structures: aorta, vertebrae, or trachea.
Regional lymph nodes
Nx Regional lymph nodes cannot be assessed;
N0 No metastases in regional lymph nodes;
N1 Involvement of 1–2 regional lymph nodes;
N2 Involvement of 3–6 regional lymph nodes;
N3 Involvement of 7 or more regional lymph nodes.
Distant metastases
M0 No distant metastases;
M1 There are distant metastases.
The following groups of lymph nodes are regional:
- disgruntled;
- internal jugular;
- upper and lower cervical;
- cervical paraesophageal;
- pretracheal (bilateral);
- lymph nodes of the lung root (bilateral);
- upper paraesophageal (above v. azygos);
- bifurcation;
- lower paraesophageal (below v. azygos);
- posterior mediastinal;
- diaphragmatic;
- perigastric (right and left cardiac, lymph nodes, along the lesser curvature, along the greater curvature, suprapyloric, infrapyloric, lymph nodes along the left gastric artery).
Category pN0 can be established only after lymph node dissection with pathomorphological examination of at least 7 removed lymph nodes (in the absence of metastases in them).
Clinical presentation and diagnosis of pharyngoesophageal diverticulum.
Small diverticula are manifested by a sore throat, dry cough, foreign body sensation, and increased salivation. When it is filled with food, swallowing problems (dysphagia) may develop. A protrusion may appear in the neck, especially when the head is pulled back. As the size of the diverticulum increases, spontaneous reflux of undigested food appears from the lumen of the diverticulum into the esophagus. As a result of compression of the trachea, difficulty breathing may occur, and when the recurrent nerve is compressed, hoarseness may occur. When food is retained for a long time in the diverticulum, a putrid odor from the mouth appears. All these manifestations lead to eating disorders and weight loss.
Puchkov K.V., Ivanov V.V. and others. Technology of dosed ligating electrothermal effects at the stages of laparoscopic operations: monograph. - M.: ID MEDPRACTIKA, 2005. - 176 p.
Puchkov K.V., Bakov V.S., Ivanov V.V. Simultaneous laparoscopic surgical interventions in surgery and gynecology: Monograph. - M.: ID MEDPRACTIKA, 2005. - 168 p.
Puchkov K.V., Rodichenko D.S. Manual suture in endoscopic surgery: monograph. - M.: MEDPRACTIKA, 2004. - 140 p.
Zenker's diverticula can be complicated by the development of diverticulitis (inflammation of the wall), then phlegmon of the neck, mediastinitis, development of an esophageal fistula, etc. Regurgitation (reflux) and aspiration (entry into the respiratory tract) of the contents of the diverticulum lead to chronic bronchitis, repeated pneumonia, and lung abscesses. Bleeding from the eroded mucous membrane of the diverticulum may occur, as well as the development of polyps and mucosal cancer.
Diagnosis of Zenker's diverticula.
Pharyngeal-esophageal diverticula can sometimes be detected by inspection and palpation of the neck. The protrusion has a soft consistency, decreases with pressure; after drinking water, a splashing noise can be detected by percussion over it.
The main diagnostic method is a contrast X-ray examination, which establishes the presence of a diverticulum, the width of the neck, the duration of barium retention in it, the degree of obstruction of the esophagus, signs of the development of a polyp and cancer in the diverticulum, the formation of esophageal-bronchial and esophageal-mediastinal fistulas. Fiberendoscopic examination makes it possible to establish the presence of a diverticulum, detect ulceration of its mucous membrane, the presence of bleeding, and diagnose a polyp or cancer in the diverticulum. Due to the high risk of perforation of the esophageal diverticulum, esophagoscopy should be performed with great caution.
It is optimal to perform esophagomanometry - a study of esophageal motility. Patients with coronary symptoms undergo a consultation with a cardiologist, an ECG study, Holter monitoring, and echocardiography.
Differential diagnosis of esophageal diverticulum is carried out with GERD, esophagospasm, hiatal hernia, esophageal strictures, achalasia cardia, esophageal cancer, mediastinal cyst, angina pectoris, and ischemic heart disease.
Treatment of esophageal diverticula
If the diverticula are small in size, there are no complications, and there are absolute contraindications to surgical treatment, conservative therapy is carried out aimed at preventing the retention of food masses in the diverticulum and reducing the possibility of developing diverticulitis.
Conservative therapy includes adherence to nutrition and diet. Food should be warm, pureed, and not irritate the mucous membrane. It is advisable to eat food in fractional portions, up to 6 times a day. After each meal, the patient drinks up to 100-200 ml of mineral water or other heated liquid and performs postural drainage of the diverticulum (drainage by body position). If esophagitis is present, drug therapy is added.
Surgical treatment of pharyngeal-esophageal (Zenker) diverticula.
Indications for surgical treatment are as follows: complications (perforation, penetration, bleeding, stenosis of the esophagus, cancer, development of fistulas), large diverticula complicated by at least short-term retention of food masses in them, long-term retention of food in the diverticulum, regardless of its size. Ineffectiveness of conservative therapy.
The essence of surgical treatment is complete removal of the diverticulum.
(cutting off from the esophagus, followed by suturing the organ wall) - diverticulectomy: the diverticulum is isolated from the surrounding tissues to the neck, a myotomy is performed, it is excised and the hole in the wall of the esophagus is sutured.
We isolate pharyngoesophageal diverticula from the cervical approach. A cosmetic skin incision is made in the projection of the anterior edge of the left sternocleidomastoid muscle. We mobilize the left lobe of the thyroid gland, retract it medially, and the neurovascular bundle laterally. Before surgery, a thick probe is inserted into the esophagus, which greatly facilitates the surgical treatment of esophageal diverticula. Then we perform extramucosal esophagomyotomy
several centimeters long, making sure that all the fibers of the m. cricopharyngeus (cricopharyngeal myotomy). We isolate the diverticulum up to the neck and stitch its base with an EndoGia-30 endoscopic stapler (Switzerland). The specimen is sent for pathohistological examination. The duration of stay in the clinic is 2-3 days. You can eat after 1-2 days.
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
Contraindications
X-ray of the stomach with barium is contraindicated in the following cases: disturbances in the functioning of the hematopoietic system, a pathological condition associated with clouding of the lens of the eye, affecting visual acuity, oncopathology of the bronchopulmonary system, carrying a child at any stage, endocrine pathologies of the thyroid gland. There are available for X-ray examination of the intestine the following contraindications:
- intestinal perforation;
- unconsciousness of the patient;
- general serious condition of the patient;
- nonspecific ulcerative colitis;
- a combination of segmental or total dilatation of the colon against the background of signs of systemic toxicity;
- severe diseases of the cardiovascular system;
- complete disruption of the passage of contents through the intestines;
- internal bleeding;
- severe pain in the epigastric region;
- pregnancy.
Epiphrenic diverticula
Epiphrenic diverticula, usually pulsational, are located along the posterior or right wall of the esophagus 2-11 cm above the diaphragm. Diverticula are spherical or mushroom-shaped. The leading factors in the formation of epiphrenic diverticula are the following factors: weakness of the muscular wall, increased intra-esophageal pressure and pressure of the food bolus on weak areas of the esophageal wall. Muscular weakness can be congenital or acquired. An increase in intra-esophageal pressure occurs due to uncoordinated peristalsis of the esophagus and its lower sphincter.
results
- abnormalities in the structure of the digestive tract;
- acute expansion or narrowing of the lumens of the stomach/esophagus;
- malformations of certain organs of the gastrointestinal tract;
- hypertonicity/hypotonicity of the muscular wall of the stomach;
- tumors, papillomas, foreign bodies;
- reduction or radial arrangement of shell folding;
- cicatricial changes at the site of tumors, ulcers, chemical burns;
- pathological narrowing;
- saccular protrusions and elasticity of the walls;
- the introduction of one section of the intestine into another with the possible development of gastrointestinal obstruction;
- intestinal motor function;
- the presence of ulcerative and inflammatory processes;
- tumors, polyposis.
An examination can show how the bauhinium valve functions. This is the structure that separates the small and large intestines and is responsible for passing food between them. If it has pathological changes, then the food gets back access, and this poses a danger to the patient’s life.
Symptoms and clinical manifestations of epiphrenic diverticula
Almost half of epiphrenic diverticula are detected incidentally as a radiological finding. Usually these are diverticula with a diameter of up to 2-3 cm. With epiphrenic diverticula, patients complain of a feeling of heaviness, pain in the lower part of the sternum or in the area of the xiphoid process, and progressive difficulty swallowing. Some patients experience aerophagia, putrid breath, and regurgitation of old decomposed food. In some cases, attacks of bronchial asthma and angina may occur. The severity of the symptoms of the disease depends on the size of the diverticulum and the degree of its filling with food masses.
Indications for surgical intervention for epiphrenic diverticula do not differ from the treatment of Zenker's diverticula. The operation is indicated for complications: perforation, penetration, bleeding, stenosis of the esophagus, cancer, development of fistulas, large diverticula complicated by at least short-term retention of food masses in them, long-term retention of food in the diverticulum, regardless of its size. Lack of effectiveness from conservative therapy.
Very important! A feature of my approach to choosing treatment tactics for patients with esophageal diverticula is the earlier determination of indications for surgical treatment using the laparoscopic method (through several punctures of the abdominal wall), without waiting for complications to develop and without wasting time on useless conservative treatment methods.
Typically, the traditional approach, which most clinics use, to epiphrenic diverticula is to perform a left-sided thoracotomy along the VII - VIII intercostal space.
Currently, in the surgery of esophageal diverticula, methods for their removal using video thoracoscopic or laparoscopic (which is even less traumatic) techniques are becoming increasingly widespread.
My experience in treating patients with esophageal diverticula is more than 14 years
.
During this time, I was able to successfully operate and treat more than 100 patients
.
Very important! Unlike other clinics, I use a minimally invasive laparoscopic approach, which allows, without opening the pleural cavity, to isolate the epiphrenic diverticulum at a distance of up to 8-10 cm from the cardia, remove it and reliably close the esophageal wound. To do this, I stitch the base of the diverticulum with an endoscopic stapler EndoGia-30 (Switzerland), which allows you to apply a 3-row titanium suture.
The basis of a precision technique for bloodless isolation of a diverticulum from surrounding tissues is the use of the LigaSure dosed vessel ligation system (Switzerland).
Very important! I always remove the esophageal diverticulum under the intraoperative control of fibroesophagoscopy; this allows during the operation (by means of illumination) to give the surgeon an excellent reference point in the surrounding tissues and, most importantly, to excise the diverticulum under double visual control (laparoscopy and fibroisophagoscopy). This double control, in turn, guarantees the completeness of its excision and the absence of narrowing of the lumen of the esophagus after suturing the diverticulum stalk with a stapler.
In the case of a combination of epiphrenic diverticula and achalasia cardia, hiatal hernia, chronic reflux esophagitis
I perform simultaneous simultaneous surgical intervention: diverticulectomy and correction of the hiatal hernia or cardiomyotomy in my own modification.
The patient begins to walk the next day after surgery and eat food 1-2 days later. Discharged on the 3rd day, after a control chest x-ray.
Thus, the earlier (before complications develop) surgery is performed for esophageal diverticulum, the better the treatment results.
Pharyngeal-esophageal diverticula are operated on by a thoracic surgeon using access to the neck, through a cosmetic incision using the LigaSure dosed vascular ligation system (Switzerland) to isolate the diverticulum and the endoscopic stapler EndoGia-30 (Switzerland), which allows you to apply a safe 3-row titanium suture to the wall esophagus.
Rice. 2. Removal of esophageal diverticulum using an endoscopic stapler using laparoscopic access.
Epiphrenic diverticula (from 1 to 10 cm from the cardia) I operate laparoscopically
through punctures, also using the LigaSure dosed vessel ligation system (Switzerland) to isolate the diverticulum and the EndoGia-30 endoscopic stapler (Switzerland) (Fig. 2).
In this case, I perform all stages under double visual control - laparoscopic and fibroesophagoscopic from the side of the lumen of the esophagus.
All of the above measures make it possible to perform surgical interventions for esophageal diverticula reliably, with a minimum number of complications, with a short hospitalization period and a quick return to normal life.
Preparation
In order for the procedure to be successful and give reliable results, it is necessary to properly prepare for an X-ray of the stomach with barium. This is a mandatory condition, if not met, the radiologist may refuse to perform the diagnosis. Preparation for an x-ray of the stomach should begin 3 days before the scheduled examination and includes the following. It is necessary to adhere to a certain diet, which involves excluding from the diet foods that cause increased gas formation (legumes, sauerkraut, black bread, fresh fruits and vegetables, whole milk). On these days, you need to eat low-fat food, steamed or boiled/baked. 12 hours before the scheduled x-ray examination, you must completely abstain from food. The procedure is performed exclusively on an empty stomach. Some patients are advised to cleanse the intestines with an enema and gastric lavage. Drinking alcohol and smoking before the examination is strictly prohibited. Immediately before the procedure in the X-ray room, the patient takes off clothes with metal fittings, jewelry, removable dentures, etc., which can negatively affect the quality of the images. An X-ray of the small intestine will also be most effective if the patient prepares for it correctly. The subject must adhere to a strict diet three days before the procedure, which will prevent flatulence and fermentation in the intestines. The doctor who sends the patient for such an examination, as a rule, explains what needs to be excluded from the diet and gives the patient a reminder. If the patient suffers from chronic constipation, then he will need to use laxatives and try to drink more clean water without gas. Colon cleansing must be done in the evening the day before the scheduled x-ray. This is done in the classical way using a series of enemas, which are also repeated on the day of the examination or using special pharmaceutical preparations - microenemas. The day before the examination, you should completely give up your usual food. Allowed to drink are broths, herbal teas, clear fruit juices. Before the procedure, it is recommended to refrain from smoking and alcohol for at least 7 days.
Postoperative follow-up
After the operation, 3-4 incisions 5-10 mm long remain on the skin of the abdomen. From the first day, patients begin to get out of bed, drink, and on the second day take liquid warm food. Discharge from the hospital is carried out on 3-4 days, depending on the severity of the disease. The patient can begin work in 2 - 3 weeks. A strict diet should be followed for one and a half to two months, a softer diet should be followed for 2-3 months. Further, as a rule, the patient leads a normal lifestyle - without medications or diet.
At the request of patients, the clinic can undergo a full examination before surgery to determine the optimal treatment tactics and choose the method of surgical intervention.
Disease prognosis
As with other cancer pathologies, survival and the possibility of cure depend on the time of detection of the tumor. Esophageal cancer is one of the most difficult to treat. In general, with late diagnosis and lack of therapy, life expectancy from the moment of diagnosis is no more than 5-7 months. If detected early - up to 6-7 years.
The survival prognosis depends on the location of the tumor and the presence of metastases. When carrying out complex therapy (surgical treatment and radiation/chemotherapy), survival rate of more than 5 years is:
- when cancer is detected at stage I – 80-90%;
- on II – 40-50%;
- at III – 5-10%.
New treatment methods are helping to increase the life expectancy of patients. The use of stereotactic radiosurgery (cyberknife) in combination with radiation therapy at a linear accelerator increases survival by 25%. A radical radiotherapy program with differentiated irradiation of the primary tumor, zones of perifocal infiltration, as well as regional metastasis pathways, increases survival for all stages of esophageal cancer by 15%.
For inoperable tumors, radiation therapy is used, which can increase life expectancy to 12 months in 10% of patients.