October 20, 2021
Bone marrow transplantation is a treatment method that is used for various blood diseases, mainly of an oncological nature. Its relevance is constantly growing, since, according to WHO data, up to 600 thousand people fall ill with leukemia and lymphoma alone every year. To date, the number of transplantations performed in the world is approaching 2 million.
Bone marrow transplantation - what is it?
Bone marrow transplantation (BMT) is a procedure for implanting healthy hematopoietic cells into the patient’s body in order to resume the process of hematopoiesis.
Indications for transplantation:
- Anemia
- All types of leukemia
- Myeloma
- Certain cancers (for example, testicular cancer)
- Hodgkin's disease
- Non-Hodgkin's lymphomas
Contraindications for transplantation:
- Severe pathologies of the liver and kidneys
- Infectious diseases
- Pregnancy
- Physical weakness of the body (old age, concomitant diseases)
Bone marrow transplantation for children is performed according to the same indications and contraindications as for adult patients.
4. Bone marrow engraftment
It takes 2-4 weeks until the transplanted stem cells take root in their new body and begin to work, producing blood and restoring lost immunity. During this entire period, the main task is, in the literal sense of the word, to preserve the life of the patient.
. High doses of chemotherapy before transplantation completely destroy the immune system; the composition of the blood almost does not allow the body to independently fight infections and prevent bleeding. A number of regular procedures are aimed at maintaining vital functions: blood transfusions, prophylactic antibiotics, constant administration of drugs that reduce the risk of rejection of new bone marrow.
Emergency aseptic measures
, if possible, eliminating the introduction of viruses and bacteria into the room. Visits, objects and food given to the patient are strictly limited. If the patient needs to leave the room, he or she puts on gloves, a gown and a mask to reduce the risk of infection in a non-sterile environment. The air in the room is constantly filtered and cleaned.
Every day, blood tests are taken from the patient to monitor the processes of bone marrow engraftment and the dynamics of blood cell production. As new stem cells begin to perform their functions, rehabilitation procedures are gradually canceled and the level of isolation from the environment decreases.
The entire rehabilitation period lasts from 4 to 8 weeks
. Most of the time, the patient’s condition remains quite serious: nausea, severe weakness, diarrhea, fever, ulceration of the mucous membranes, bleeding. The feeling is similar to the symptoms of the flu, only very prolonged, which in itself depletes the already weakened body. The condition from day to day can range from satisfactory to very severe. For all painful and dangerous manifestations, urgent symptomatic medical care is provided.
When tests show that bone marrow engraftment was successful and the patient no longer needs supportive and rehabilitation procedures, the doctor decides to discharge the patient. As a rule, within a year from this moment a person cannot return to a state of full functionality.
. He is very weak and must visit the hospital regularly for blood checks, certain medications and even blood transfusions, since during this period the level of essential blood cells can be greatly reduced. Visiting places with large crowds of people is not recommended; a full active life and usual activities are not possible until full restoration of strength occurs and stability in the functioning of the new bone marrow is achieved.
It should be noted that, despite the severity of the procedure and all the dangers of the recovery period, a successful bone marrow transplant saves lives and significantly restores the quality of life. Finding themselves on the brink of a seemingly inevitable death and having “miraculously” avoided it, many recovering people reevaluate their attitude towards the world, rediscovering what is truly important.
What types of transplants are there?
It is customary to distinguish between the following types of bone marrow transplantation:
- Autologous transplantation is an operation in which the patient is implanted with his own cells.
- Allogeneic transplantation from a relative
- Allogeneic transplant from an unrelated donor
- Haploidentical transplantation is a type of transplant that uses the bone marrow of a partially compatible relative. Graft survival after this procedure occurs in only 25% of patients
Suitability for transplantation
Stem cell transplantation is best tolerated by younger people and patients who have just started treatment. Some transplant centers set age limits. For example, traditional allogeneic transplantation (there are several types of this procedure) is often offered only to patients under 50 years of age, and autologous transplantation to patients under 65 years of age. Stem cell transplantation may be contraindicated if you have severe heart, lung, liver, or kidney disease. Some of these patients are given what is called a mini-transplant.
How do you prepare for transplantation?
Preparing the patient for transplant
The most important stage of preparation for transplantation is conditioning. This is a therapy used for cancer. It consists of taking chemotherapy drugs and immunosuppressants. This suppresses the patient’s immunity to prevent rejection of the transplanted material. The method also helps destroy cancer cells and frees up space for the transplant.
In the case of transplantation of one's own cells, a collection is first made, and then the material is frozen until the end of the chemotherapy course.
Diagnostic procedures before bone marrow transplant surgery:
- Consultations with specialists, incl. dentist
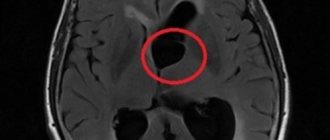
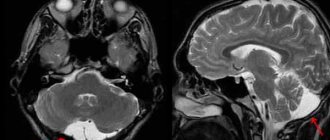
- MRI and CT, PET-CT (if we are talking about cancer)A
- blood test (including for HIV, hepatitis, etc.)
- A biochemical blood test is performed to ensure that the liver and kidneys are functioning properly. Otherwise, transplantation may be contraindicated
- Trephine biopsy and bone marrow aspiration. This is a puncture of bone tissue and bone marrow followed by cytogenetic analysis
If necessary, the patient undergoes treatment at the dentist. This is necessary to completely eliminate infections, since after transplantation their presence is deadly.
Preparing for donation
The donor undergoes routine testing to rule out any diseases that could be passed on to the recipient.
If the sample is taken from peripheral blood, the donor is prescribed special medications that must be taken for 5 days. They promote the active release of cells into the bloodstream.
There may be side effects from taking these medications. Usually these are short-term bone pains.
Side effects of infusion
Side effects from the infusion are rare and usually not dangerous. Many of these side effects are caused by the preservative used when freezing stem cells (dimethyl sulfoxide, or DMSO). For example, your mouth may taste strongly of garlic or corn in a creamy sauce. Sweet candies or flavored drinks, which can be consumed both during and after the infusion, will help to cope with it. A specific smell can envelop the entire body. It often causes discomfort to others, but the patients themselves, as a rule, do not even notice it. The smell and taste persist for several days, after which they gradually disappear. If the room smells of garlic or corn, you can place chopped oranges in it. Patients who received stem cells that were not frozen do not complain of this problem, since the stem cells are not mixed with a preservative during processing.
There are other side effects known to occur in some patients both during and immediately after a stem cell transplant. These side effects include:
- fever or chills;
- shortness of breath;
- hives;
- feeling of tightness in the chest;
- low blood pressure;
- cough;
- chest pain;
- decrease in urine volume;
- weakness.
Again, the above side effects are rare and minor. If any side effects occur, the patient is prescribed appropriate treatment. In any case, the stem cell infusion must be completed.
How is transplantation performed?
Stage 1. Fence
Bone marrow is collected under general anesthesia. First, the doctor makes a small incision and then uses a wide needle to puncture material from the femur.
The donor can also choose to collect cells from peripheral blood. To do this, the donor is connected to a machine that pumps blood for several hours. Through a special separator, bone marrow cells are separated from the blood and collected in a separate reservoir.
Stage 2. Transfer
Bone marrow is transplanted by intravenous injection. The procedure lasts up to 2 hours.
Stage 3. Engraftment period
The injected cells eventually take root and begin to produce new healthy blood cells.
Hospitalization lasts about 3 months.
Send a request for treatment
Who can become a donor for a bone marrow transplant?
The related donor can be the patient's sibling. However, even such a donor is not always compatible. In rare cases, a haploidentical transplant is performed. The donor can be the patient's father or mother.
For an unrelated transplant, candidate selection occurs through the bone marrow donor bank database. The search usually takes about 2 weeks. The largest are the US Bone Marrow Donor Bank, European and German banks. Usually 2-3 people are selected, since a potential candidate may have temporary contraindications, refuse the procedure, or may not be in the country.
It is worth noting that there are times when it is not possible to find a suitable candidate.
Contraindications to donation are:
- Infectious diseases
- Autoimmune diseases
- Mental disorders
- Age under 18 and over 55 years old
2. Bone marrow compatibility, obtaining bone marrow from a donor
Bone marrow compatibility
The treatment regimen using donor bone marrow includes two stages:
- destruction of diseased cells of one’s own bone marrow;
- transplantation of healthy stem cells from a donor.
The main problem for every bone marrow transplant candidate is finding a donor.
. The most favorable prognosis is if the stem cells are obtained from a close relative (ideally a twin). If there is no person suitable for donation among your relatives, you have to look in the international registry of bone marrow donors. The genetically closer the donor's cells are to the recipient's cells, the less likely it is that the body will perceive it as foreign and begin to reject it. It is even more dangerous if the transplanted material itself turns on immune defense and begins to attack its new host.
Sometimes the material for transplantation can be the patient's own bone marrow. This operation is called "autotransplantation"
, is possible in a number of malignant tumors localized in diseased organs, but not yet affecting the bone marrow. Sometimes they resort to filtering their own stem cells from those affected by the disease in order to obtain material suitable for autoimmune transplantation.
Receiving bone marrow from a donor
Depending on the height and weight of the recipient awaiting transplantation, the required amount of donor material can range from 950 to 2000 ml
. Bone marrow collection occurs under general anesthesia, although it does not require any skin or tissue incisions. Through punctures in the pelvic and femur bones, the bone marrow mixed with blood is removed from the donor in several stages with a syringe. After the procedure for collecting bone marrow, there may be pain at the puncture sites, as if after a blow to the bone, but usually, upon recovery from the state of anesthesia, no unpleasant sensations remain, and within a few weeks the volume of the donor’s bone marrow is completely restored.
If necessary, the collected material is examined, cleaned and frozen.
Visit our Oncology page
What complications can there be after the procedure?
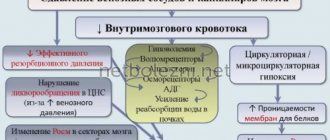
The most serious complications after bone marrow transplantation are rejection of the graft by the body and attack of the transplanted cells on the patient's body (graft-versus-host disease). To prevent both of these reactions, the patient is prescribed immunosuppressants - drugs that suppress the immune system.
Such therapy, in turn, exposes the patient’s body to the risk of infection. In order to minimize this risk, the patient is placed in a sterile box. This is an isolated sterile room equipped with antibacterial filters.
There is no risk of complications for the donor during a bone marrow transplant. However, there are minor side effects. Possible feelings of weakness and nausea. Hospitalization of the donor lasts one day. Pain at the puncture site disappears after a few days. The donor's bone marrow cell volume is restored after 2 weeks.
The consequences of transplantation for the patient depend on a number of factors:
- Initial diagnosis
- Levels of donor compatibility
- Relative physical health
- Compliance with the isolation regime during the engraftment period
- Competent treatment protocol
If all the necessary precautions are followed and the treatment is carried out in a well-equipped center under the guidance of an experienced doctor, the chances of recovery are high. This also applies to patients with malignant diseases.
Types of procedure
Nowadays, two methods of hematopoietic stem cell transplantation are actively used, which are fundamentally different in the direction of action - autologous and allogeneic. In the first case, the same person plays the role of donor and recipient, and the main condition is the absence of bone marrow damage. In the second, a careful selection of the person closest to the patient in terms of alleles - paired genes - takes place.
- Autologous bone marrow transplantation can be used as a treatment for various forms of oncology, provided there are no metastases in the pelvic and femoral bones. The technique has also shown high effectiveness in the treatment of multiple sclerosis and rheumatoid arthritis. First, the patient undergoes a procedure for collecting hematopoietic cells, and after 10-15 days receives the introduction of his own stem material. This allows you to restore the protective mechanisms of the leukocyte system, eliminating “shielding”, in which the immune system is not able to recognize the tumor.
- Allogeneic bone marrow transplantation is performed in cases where the patient's bone marrow already has an altered genotype - in case of leukemia, hereditary pathologies of hematopoiesis. This method requires a donor - a person whose tissues have a similar genotype. A prerequisite is the absence of diseases such as viral hepatitis, tuberculosis, malaria, oncology, HIV and mental disorders on the card.
How is rehabilitation after blood-forming cell transplantation?
Conclusions about the success of the transplant can only be made after several weeks after the operation. During this time, the transplant takes root in the patient's body. During the period of graft engraftment, the patient is prescribed maintenance therapy in the form of antiviral and antifungal drugs, as well as antibiotics.
A bone marrow transplant requires recovery not only physical, but also psychological. The patient experiences severe weakness for a long time. This condition affects his mental well-being, so it is extremely important to receive professional help from a psychologist during this period. It is also necessary for the patient's family to support him during this time.
Life after bone marrow transplant
The life of transplant patients is not much different from the everyday life of an ordinary person. For some time it is necessary to follow the doctor’s instructions, but this does not significantly affect the quality of life.
What is the prognosis for life after transplantation?
Survival after bone marrow transplantation depends primarily on the initial diagnosis. Also, the experience of the oncohematologist who transplants the cells is important. Thus, in German and Turkish clinics, the average survival rate of patients after transplantation is more than 90%.
It is impossible to determine the life expectancy after a bone marrow transplant, since this indicator depends on many factors. A person is considered completely cured after surviving 5 years after the procedure.
Relapse after bone marrow transplant
There is a possibility of relapse after a bone marrow transplant. This figure varies significantly depending on the clinic where the procedure is performed. Thus, in foreign bone marrow transplant centers, the statistics of relapse are much lower than the same indicator in CIS clinics.
The more time has passed since the transplant, the lower the likelihood of relapse. If the disease returns, the transplant is repeated. The risk of disease-free survival after a second transplant depends on the time interval between the first transplant and the first relapse. If this period lasted more than a year, the chances of recovery are high.
Rehabilitation
Despite the technical simplicity of the transplant, the patient remains in the clinic for about two weeks, because strict medical supervision and a sterile environment are necessary conditions for successful rehabilitation. During the preparation process, the immune system is completely suppressed and the patient has an increased susceptibility to viruses and microbes that surround him in everyday life.
After successful engraftment of the transplanted cells, the patient quickly recovers - blood counts normalize, tumors decrease and metastases disappear. For leukemia, transplantation is the most effective method of therapy.
Where is bone marrow transplant surgery performed?
Booking Health has identified for you the 2 best, in our opinion, clinics for bone marrow transplantation in leading countries.
Germany
The leading German clinic in the field of hematopoietic cell transplantation is the University Hospital Ulm. The Department of Hematology, Oncology, Palliative Medicine, Rheumatology and Infectology is part of the Comprehensive Cancer Center Ulm and is certified by the German Cancer Society and the German Cancer Organization.
Türkiye
One of the leading Turkish clinics in the field of oncohematology is Memorial Sisli Hospital, Istanbul. The Department of Pediatric Hematology and Bone Marrow Transplantation at Memorial Şişli Clinic performs all types of bone marrow transplantation in children. The head physician of the department, Professor Atilla Taneli, is a member of the European Society for Bone Marrow Transplantation and the JACIE organization for the accreditation of medical institutions involved in bone marrow transplantation.
The transplantation process involves a large number of steps, from the initial decision to undergo transplantation through pre-transplant patient assessments, internalization and long-term follow-up after discharge.
Before the transplant procedure, the coordinator will provide the patient with detailed information with answers to all questions about the process, as well as the date and time of the initial assessment consultation at the clinic. The transplant specialist informs the patient about the possibility of complications, success rates, and long-term results. This examination will be the starting point of the transplantation process. The patient will be asked to give written consent for the operation. After this, preparatory studies begin.
Initial assessment
For the initial assessment, the patient must have a consultation with a bone marrow transplant specialist at the Bone Marrow Transplant Center outpatient clinic. Consultation includes:
- The doctor examines the patient’s medical history (anamnesis), the treatment received, discusses treatment options and provides the patient with information about the recommended treatment;
- Inspection of the ICA Bone Marrow Transplantation Center accompanied by a nurse coordinator;
- The nurse coordinator refers the patient to a special department for referral or medical insurance. After signing the consent for bone marrow transplantation, the following steps are taken:
Planning
Selecting an accompanying person: A relative or close friend is selected to assist the patient in all situations, including monitoring the patient's health, physical assistance, obtaining and administering medications, performing administrative procedures for the clinic, maintaining contact with the doctor and nurse, and emotional and psychological support. The Center Nurse Coordinator will inform the selected individual of his/her responsibilities and provide training.
Accommodation: The patient will be informed of the need to rent housing in the immediate vicinity of the MCA 1-4 months before transplantation. A team of patient/international patient relations specialists will assist in organizing the process.
Financial preparation: financial expenses are planned for the entire transplantation process.
Preparation for transplantation
Donor selection
Allogeneic Transplantation: The first step in allogeneic transplantation is the selection of an HLA-matched sibling or relative.
Autologous transplantation: The donor is the patient of autologous transplantation. Depending on the patient's health and diagnosis, the team of specialist doctors at the Bone Marrow Transplant Center will determine the type of bone marrow mobilization, as well as the time and method.
Donor examination in Medical: the donor (the patient himself, a relative, etc.) undergoes an initial examination in the clinic.
First consultation: The doctor and nurse will examine the patient at the Bone Marrow Transplant Center clinic to obtain medical history, conduct examinations and blood tests, and introduce the patient to the clinic.
Consulting the donor and the patient's relatives: The next day, the doctor and nurse make an appointment to meet with the patient and his family/friend to explain the transplant process, its benefits and risks, and answer all questions.
Examination: Outpatient examinations will be carried out over 1-2 weeks. These examinations are aimed at establishing the general state of health. Additional examinations such as bone marrow aspiration, chest X-ray, ECG are performed if necessary.
Consultation on the results of the examination: the doctor will inform the patient about the results of the examination and tests, answer all questions and explain the current situation.
Education: the patient and accompanying person will be told about the transplantation process, the operation in the clinic and the patient’s condition after discharge.
Donor: The donor will also be informed on all issues, and he/she will also be given the opportunity to ask questions if he/she is a relative. If it is necessary to collect bone marrow from a donor, the material will be collected and frozen in accordance with the previously established regime.
During autologous transplantation, peripheral blood stem cells will also be collected and frozen in accordance with the established stem cell mobilization regimen. The process of bone marrow mobilization lasts from 7 to 20 days, depending on the chosen regimen.
Preparatory mode
At the clinic, the patient will undergo chemotherapy and/or radiation therapy in accordance with an individualized treatment plan in order to completely (myeloblastic transplants) or partially (reduced-intensity or non-myeloblastic transplantations) destroy the bone marrow cells. The duration and type of treatment vary depending on the type of disease. Typically the duration of treatment is from 2 to 8 days. This treatment regimen will weaken the immune system, making the patient more vulnerable to infections. Treatment may also cause side effects such as nausea, difficulty swallowing, abdominal pain, fatigue and loss of appetite. Preventive measures will be taken to minimize discomfort.
Stem cell transplantation
1-2 days after completion of the preparatory regimen, a stem cell transplant is performed, which is very similar to the blood transfusion procedure.
Regardless of whether the transplantation is allogeneic or autologous, frozen bone marrow or peripheral blood stem cells taken from the donor will be thawed and, after the necessary preparation, administered intravenously to the patient through a central catheter.
Bone marrow or peripheral blood stem cells can be collected from a donor and infused into the patient without being frozen. In this case, the donor's mobilization regimen will begin before transplantation. The bone marrow is collected directly on the day of transplantation and administered intravenously to the patient without freezing.
Bone marrow is collected from the donor in the operating room on the day of transplantation and immediately injected into the patient. This method is usually used when working with patients suffering from aplastic anemia and chronic myeloid leukemia.
Engraftment process
Engraftment is the successful integration of transplanted bone marrow into the patient’s body, which is expressed in the reproduction of blood elements. This process takes from 10 to 35 days. The most serious complications that can occur during this period are infection and bleeding. Neutrophil engraftment is an increase in the number of neutrophils to more than 500 over the next two days. Platelet engraftment—platelet count increases to more than 20,000 over the next two days. Neutrophil engraftment time can be reduced by 2-3 days by using a growth factor called G-CSF (granulocyte colony-stimulating factor). During this period the patient will be hospitalized. After the engraftment period, the patient's status and discharge date will be determined based on factors such as absence/presence of infections, absorption of intravenous medications, and proper self-feeding.
Recovery after engraftment
The first signs of recovery after engraftment can be seen after about 3 months. This period will need to be spent near the clinic in Istanbul. The patient will need to visit the MCA regularly for blood tests (every week or more often). The person accompanying the patient must be ready to help the patient in everything during this period. Before the process begins, the patient and accompanying person will undergo special training to learn everything. If you have any questions or complications during this period, you will be able to contact your doctor or nurse by telephone at any time. The time intervals between regular checks will increase as the patient begins to recover.
Long-term follow-up after recovery
Once engraftment is complete, the healing process begins. The patient and his accompanying person will be informed about the need for long-term observation. The patient will undergo a detailed examination and receive a conclusion. During the next consultation with the doctor and nurse, the patient and his accompanying person will be provided with comprehensive information about further actions, cases that require special attention, lifestyle, diet and physical activity. Despite the fact that the patient will have all this information, the doctor will still monitor the patient’s condition for a long time. The first time the patient is invited for examination is after three months. For each patient, an individual long-term follow-up plan is drawn up depending on the medications taken, the degree of restoration of the immune system, graft-versus-host disease, and possible complications. Patients are also encouraged to participate in a vaccination program at 12 and 24 months after engraftment.
How much does a bone marrow transplant cost?
Transplant prices in German clinics start from €212,000. At the same time, a transplant from an unrelated donor will cost more, since the search for a donor is paid separately.
Transfer prices in Turkey start from €97,000. The price depends on the type of transplant, diagnosis and general condition of the patient.
The price of a bone marrow transplant for children in any country may vary slightly. In addition, some foreign centers perform transplants for children only after full prepayment of the medical program.
Send a request for treatment
Organization of bone marrow transplantation abroad
If a bone marrow transplant is necessary, a number of questions arise. In which country should I have a transplant? Do you need a visa? Is prepayment required? Is it possible to go urgently for treatment? Where to find a donor? How to get to the best specialist?
In order to resolve all these issues, contact the Booking Health manager. Our specialists will choose the best solution for you.
Our advantages:
- Individual selection of a clinic
- Possibility of choosing the best doctor
- Services: provision of transfer and interpreter, preparation of medical documentation
- Insurance that will ensure that the stated price is maintained. We will cover all unexpected expenses