Stomach ulcer, its types and stages
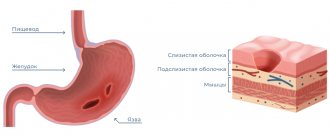
Gastric ulcer (hereinafter referred to as PUD) is a disease in which a mucosal defect occurs and the submucosal layer may be affected. This is a chronic disease that occurs in waves, with periods of exacerbation and remission.
An ulcer can be localized in different parts of the stomach:
- subcardial and cardiac - in the upper part;
- antrum - in the lower section;
- in the body - in the middle part;
- in the pyloric canal - at the transition to the duodenum.
The size of the ulcer is:
- small - up to 5 mm in diameter;
- medium - in diameter 6-19 mm;
- large - 20-30 mm in diameter;
- gigantic - more than 30 mm in diameter.
There are also ulcers associated with the bacterium Helicobacter pylori (hereinafter referred to as HP) and those not associated with it.
The disease occurs in several stages:
- exacerbations - the occurrence of a defect in the mucous membrane;
- scarring - the formation of connective tissue at the site of the ulcer;
- remission - healing of the defect.
The stage of cicatricial and ulcerative deformation of the organ is distinguished separately.
General information
Gastric ulcer (GUD) is a cyclically relapsing chronic disease, the characteristic feature of which is ulceration of the stomach wall. PUD is the most common pathology of the gastrointestinal tract: according to various sources, from 5 to 15% of the world's population suffer from this disease, and among urban residents the pathology is five times more common. Many specialists in the field of gastroenterology combine the concepts of gastric ulcer and duodenal ulcer, which is not entirely correct - ulcerations in the duodenum are diagnosed 10-15 times more often than ulcers in the stomach. However, PU requires careful study and development of modern diagnostic and treatment methods, since this disease can lead to the development of fatal complications.
About 80% of cases of primary detection of gastric ulcers occur in working age (up to 40 years). In children and adolescents, gastric ulcers are diagnosed extremely rarely. Among the adult population, there is a predominance of men (women suffer from peptic ulcers 3-10 times less often); But in old age, sex differences in incidence are smoothed out. In women, the disease is milder, in most cases asymptomatic, and is rarely complicated by bleeding and perforation.
Gastric ulcer ranks second among the causes of disability in the population (after cardiovascular pathology). Despite the long period of study of this nosology (more than a century), therapeutic methods of influence that can stop the progression of the disease and completely cure the patient have not yet been found. The incidence of gastrointestinal ulcers throughout the world is continuously growing, requiring the attention of therapists, gastroenterologists, and surgeons.
Main causes
The cause of a defect in the gastric mucosa is considered to be an imbalance between the aggressive secretions of the stomach and the protective qualities of the mucous membrane. To digest food, the stomach secretes pepsin and hydrochloric acid. To prevent them from destroying the stomach, mucus forms on its surface, protecting the organ. If more acid is produced and less mucus is produced, an ulcer may form. The background for such a pathology may be a decrease in gastric motility, a violation of the regenerative - restorative properties of the mucous membrane against the background of certain diseases.
The main etiological cause of ulcer formation is damage to the mucous membrane of the HP. This bacterium successfully survives in an acidic environment and produces an enzyme that causes an inflammatory reaction with subsequent formation of a defect. Helicobacter pylori is detected in 82% of patients suffering from gastric ulcers.
Another reason may be uncontrolled use of anti-inflammatory non-steroidal drugs, such as aspirin.
Provoking factors may be:
- smoking and alcohol abuse;
- constant consumption of spicy food;
- stressful situations;
- hereditary predisposition;
- dry food;
- eating disorder.
Gastric ulcers often develop against the background of certain diseases, such as atrophic gastritis and hormonal pathologies.
Symptoms of the disease
Peptic ulcer usually manifests itself more often in spring and autumn, during the period of exacerbation of the disease. The first sign of the disease is pain that occurs immediately after eating. This is due to the fact that pepsin and hydrochloric acid released during meals aggressively affect the defect unprotected by mucus. Moreover, the manifestations of pain symptoms increase within an hour after eating. The pain is localized in the epigastric region, in the region of the heart, and can radiate - radiate under the scapula, as in a heart attack. At the height of the pain syndrome, nausea often occurs, which can result in vomiting, which brings relief.
Other dyspeptic manifestations and signs of illness: heartburn, loss of appetite, constipation. A coated tongue may indicate stomach problems. Against this background, the patient quickly loses weight.
Treatment of the disease
Gastric ulcers are well treated with conservative methods, which include pharmacotherapy and physiotherapeutic procedures. In emergency and some other cases, surgical intervention is indicated.
Drug treatment
The treatment of gastric ulcers uses complex pharmacotherapy, including medications aimed at the root cause of the pathology, relieving irritation of the mucous membrane and creating a protective barrier for gastric juice and relieving pain. The main group of drugs includes:
- Proton pump inhibitors are long-acting drugs that reduce gastric secretory activity.
- Antacids - envelop the mucous membrane, protecting it from the aggressive effects of gastric juice, and reduce its acidity.
- Antibacterial drugs are aimed at eradication (destruction) of Helicobacter pylori. The best effect is achieved when antibiotics are combined. For peptic ulcers, macrolides, antiprotozoal drugs, penicillin and tetracycline antibiotics are prescribed.
- Bismuth preparations relieve inflammation and form an insoluble colloid that creates a protective film when combined with protein.
- Vitamin B5 (Pantothenate) - normalizes the production of hydrochloric acid, stimulates the regeneration of the mucous membrane.
- Methylmethionine sulfonium chloride, also called vitamin U, acts as a cytoprotector that helps reduce gastric secretion and heal gastric ulcers.
Treatment can be supplemented with other drugs aimed at eliminating the causes of ulcerative pathology.
Physiotherapy
Physiotherapy helps ulcer healing and can be used in complex therapy. The mechanisms of self-regulation and adaptation are beneficially affected by:
- laser puncture - exposure of bioactive points with a laser beam;
- EHF therapy - the influence of electromagnetic waves in the millimeter range;
- magnetotherapy - exposure to low-frequency magnetic fields.
Ultrasound therapy is used to improve gastric motility in case of gastric atony. This procedure also improves blood supply to the organ, reduces the number of bacteria and relieves inflammation.
Surgery
Emergency surgery is performed in case of massive bleeding and perforated gastric ulcer. Surgical intervention is also indicated for complicated forms of ulcers in the case of a non-healing ulcer, as well as for malignancy, when the pathology becomes malignant. In some cases, gentle methods are used: laparoscopy or endoscopy.
specialist
Our doctors will answer any questions you may have
Tumasova Anna Valerievna Gastroenterologist
Ask a Question
Diagnostics
The gold standard for diagnosing gastric ulcers is esophagogastroduodenoscopy. Endoscopy allows you to visualize the ulcerative defect in 95% of patients and determine the stage of the disease (acute or chronic ulcer). Endoscopic examination makes it possible to promptly identify complications of gastric ulcer (bleeding, cicatricial stenosis), conduct endoscopic biopsy, and surgical hemostasis.
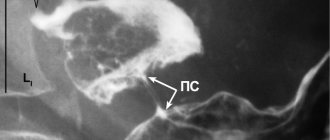
X-ray of the stomach (gastrography) is of paramount importance in the diagnosis of cicatricial complications and penetration of ulcers into nearby organs and tissues. If endoscopic visualization is not possible, radiography can verify a gastric ulcer in 70% of cases. For a more accurate result, it is recommended to use double contrasting - in this case, the defect is visible in the form of a niche or a persistent contrasting spot on the wall of the stomach, to which the folds of the mucous membrane converge.
Considering the huge role of Helicobacter pylori infection in the development of peptic ulcer, all patients with this pathology undergo mandatory tests to detect H. pylori (ELISA, PCR diagnostics, breath test, examination of biopsy specimens, etc.).
Of auxiliary importance for gastric ulcers are ultrasound of the gastrointestinal tract (detects concomitant pathology of the liver, pancreas), electrogastrography and antroduodenal manometry (makes it possible to assess the motor activity of the stomach and its evacuation ability), intragastric pH-metry (detects aggressive factors of damage), stool analysis for hidden blood (done if gastric bleeding is suspected). If a patient is admitted to the hospital with a clinical picture of an “acute abdomen,” diagnostic laparoscopy may be required to exclude gastric perforation. Gastric ulcers must be differentiated from symptomatic ulcers (especially medicinal ones), Zollinger-Ellison syndrome, hyperparathyroidism, and gastric cancer.
Diet and bad habits for stomach ulcers
Diet for gastrointestinal ulcers is an essential part of treatment. During the acute period, nutrition should be as gentle as possible, gentle on the mucous membrane and not stimulating the secretory activity of the stomach. In the first two days, preference is given to slimy soups with rice water without vegetables and meat, jelly or warm tea with sugar and crackers. In the next 6 days, table No. 1 is used in therapeutic nutrition.
Authorized Products
General nutrition rules:
- include easily digestible foods in the diet;
- food should be warm
- Do not eat cold or hot foods;
- you need to eat slowly, in small portions
- products need to be crushed and ground;
- Baking, boiling, stewing is allowed;
- fried foods and spices are excluded;
- the break in eating should not be more than 3 hours;
- food must be chewed thoroughly.
The following foods and dishes are allowed for stomach ulcers:
- Slimy soups: with the addition of rice, semolina, oatmeal, you can add cream or butter;
- Slimy porridges: with water or milk from the same cereal, you can add cream;
- Fish and meat: lean beef, veal, turkey, rabbit, chicken. To prepare the meat, you need to boil it, pass it through a meat grinder, add butter, bake it into a soufflé puree, you can cook steamed cutlets, meatballs, meatballs;
- Eggs: soft-boiled, or steam omelet;
- Berries and fruits: baked unsweetened fruits, dried fruit compotes;
- Dairy products: milk, steamed pureed cottage cheese soufflé, cream.
- Drinks: weak tea with added cream or milk, rosehip decoction, milk or fruit jelly.
You can add refined vegetable oil or unsalted butter to dishes.
Prohibited Products
During an exacerbation, foods that irritate the gastric mucosa and increase the production of gastric juice are excluded: fatty meat, baked goods, preserves, canned and smoked foods, confectionery with cream, dishes with vinegar and spices, garlic.
Do not include vegetables with coarse fiber in the diet, as well as radishes, radishes, daikon, cabbage, tomatoes, turnips, and mushrooms.
It is necessary to avoid foods that cause fermentation processes: legumes, sweet fruits and juices, carbonated drinks.
During the treatment period, you are strictly prohibited from smoking and drinking alcohol.
Modern approaches to the treatment of gastric and duodenal ulcers
At the end of the twentieth century. A significant step has been taken towards changes in the principles of treatment of peptic ulcer disease (PU). The success of modern approaches to therapy is associated primarily with the use of new antisecretory drugs and Helicobacter pylori (HP) eradication regimens. Currently, pharmacotherapy for ulcer includes more than 500 different drugs and about 1000 combinations of them. The modern concept of treatment of ulcer provides for active therapeutic tactics, including multicomponent drug regimens and long-term use of medications according to indications.
An important component of modern pharmacotherapy for peptic ulcer disease is the absence of fundamental differences in approaches to the treatment of gastric and duodenal ulcers. The basic principles of therapy for peptic ulcer disease are:
- impact on factors of aggression and/or defense;
- etiological therapy;
- correction of drug treatment taking into account concomitant diseases;
- individual characteristics of the patient (age, body weight, tolerance of medications used, activity, i.e. ability to care for oneself);
- financial capabilities of the patient.
- The main directions in the treatment of peptic ulcer disease during exacerbation include:
- etiological treatment;
- treatment regimen;
- therapeutic nutrition;
- drug treatment;
- herbal medicine;
- use of mineral waters;
- physiotherapeutic treatment;
- local treatment of long-term non-healing ulcers.
Currently, in the pathogenesis of ulcers, especially duodenal ulcers, great importance is attached to the infectious agent - H. pylori. Epidemiological data obtained in various countries indicate that 100% of duodenal ulcers and more than 80% of ulcers localized in the stomach are associated with persistent HP.
Many studies confirm that anti-Helicobacter therapy leads to a decrease in the frequency of relapses of gastric ulcer (GUP) and duodenal ulcer (DU). The strategy for treating ulcer using eradication of HP infection has undeniable advantages over therapy with all groups of antiulcer drugs, as it provides long-term remission of the disease and, possibly, complete cure. Anti-Helicobacter therapy has been well studied in accordance with the standards of evidence-based medicine [8]. Modern approaches to the diagnosis and treatment of H. pylori infection, meeting the requirements of evidence-based medicine, are reflected in the final document of the second Maastricht consensus, adopted in September 2000. The main differences between the current document and the agreement five years ago are several important points [5].
- For the first time, the treatment of H. pylori infection, and therefore the diseases associated with it, is the responsibility of a general practitioner, and not a gastroenterologist, as was previously the case. The competence of a gastroenterologist includes only those cases where treatment of the disease, including using second-line therapy, was unsuccessful, as well as cases that clearly require specialist intervention.
- For the first time, two-stage treatment was introduced: when choosing a first-line regimen, the doctor must simultaneously immediately plan reserve therapy.
- It is recommended to use anti-Helicobacter therapy in patients with functional dyspepsia, as well as in cases where long-term therapy with non-steroidal anti-inflammatory drugs is planned.
- Patients with uncomplicated duodenal ulcer are recommended to be prescribed only recommended courses of anti-Helicobacter therapy, without subsequent use of antisecretory drugs.
The main criterion for choosing anti-Helicobacter therapy is its expected effectiveness, providing a high percentage of eradication (more than 80%).
Rules and recommendations of the Russian Gastroenterological Association for the treatment of HP infection for the use of anti-Helicobacter therapy.
- If the treatment regimen used did not achieve eradication, it should not be repeated according to this regimen.
- If the regimen used does not lead to eradication, this means that the bacterium has acquired resistance to one of the components of the treatment regimen.
- If the use of one and then another treatment regimen does not lead to eradication, then the sensitivity of the HP strain to the entire range of antibiotics used should be determined.
The adoption by the Russian Gastroenterological Association in 1998 of national recommendations for the diagnosis and treatment of Helicobacter pylori infection and mass familiarization of doctors with them have not yet led to a decrease in the number of strategic and tactical errors in determining indications for eradication and choosing adequate anti-Helicobacter pylori regimens (see Table 1) [4 ].
Table 1. Errors in the treatment of HP infection.
| Errors in patient selection | Errors in treatment regimens |
|
|
What does a doctor need to know when starting anti-Helicobacter therapy? Every general practitioner, especially those with more than five years of experience, will most likely have to overcome some psychological barrier before prescribing antibiotics to a patient with a peptic ulcer. Today, gastroenterologists and therapists still have different attitudes towards anti-Helicobacter therapy for ulcerative disease. Strict, strict adherence to the anti-Helicobacter treatment regimen is necessary [10]. Their effectiveness has been proven, they correspond to the characteristics of HP and the pharmacokinetics of the drugs, and the side effects of such therapy are also known.
It is better not to carry out anti-Helicobacter therapy at all, rather than to carry it out incorrectly - since in this case, HP resistance to a number of components quickly develops. In this regard, the patient must be told in detail about the upcoming treatment and obtain his consent to cooperate with the doctor. It is also important to assess the patient’s financial capabilities. He should know that, thanks to expensive, one-time treatment, it will be possible to achieve stable remission in patients with duodenal ulcer in 70–80% of cases, and in patients with duodenal ulcer – in 50–60%, which is ultimately cost-effective.
Which eradication scheme to choose? If there is a stomach or duodenal ulcer against the background of increased acid production, then preference should be given to classic three-component regimens based on a proton pump blocker (PPI) (omeprazole, etc.). Then it is possible to switch to a single dose of PPI without antibacterial drugs. You should not use regimens containing nitroimidazoles (metronidazole, tinidazole) if you have a history of drugs from this group being prescribed for other indications.
Currently, in Russia there is a sharp increase in the number of HP strains resistant to nitroimidazoles [2, 9]. Taking this into account, the search for more effective HP eradication regimes seems to be an urgent task today. Therefore, in recent years there has been growing interest in the use of macrolides in the treatment of HP-associated diseases. Numerous studies have shown the effectiveness of using macrolide antibiotics for the treatment of HP. These drugs have a high ability to penetrate cells and are intensively released onto the mucous membranes (MS), which increases their effectiveness against HP. In addition, macrolide antibiotics have fewer contraindications and side effects, and they have a higher eradication rate than tetracyclines, which can also accumulate in cells [11]. The peculiarity of HP infection is that it is accompanied by hyperacidity.
In this regard, most macrolide antibiotics undergo increased hydrolysis and cannot be used. An exception is clarithromycin, which is resistant to hydrochloric acid [11].
Therefore, the purpose of our study was to develop new eradication therapy regimens for duodenal ulcer associated with H. pylori using omeprazole (O), as well as a combination of amoxicillin (A) and clarithromycin (K). We used the following eradication regimen - Ultop (omeprazole) 20 mg twice a day + Fromilid (clarithromycin) 500 mg twice a day + Hiconcil (amoxicillin) 1000 mg twice a day - a course of seven days. Eradication was 90%. The study showed that the use of fromilid (clarithromycin) is effective and advisable in anti-Helicobacter therapy regimens using PPIs.
Data from numerous studies and the results of their meta-analysis allowed us to conclude that the inclusion of antisecretory drugs in HP infection eradication regimens not only improves HP eradication when combined with antibiotics, but also helps accelerate ulcer scarring and allows for faster elimination of the symptoms of ulcerative dyspepsia. As for the specific mechanisms for increasing the effectiveness of eradication due to the use of antisecretory drugs, then, first of all, with an increase in the pH of the gastric contents, the minimum inhibitory concentration of antibiotics (MIC) decreases and their effectiveness accordingly increases. The viscosity of gastric juice and the concentration of the antibiotic in the gastric contents also increase, which increases the exposure time of antibacterial drugs to the bacterium H. pylori [11]. We studied the effectiveness of ultope (omeprazole) - pH > 4 of the gastric contents with a single dose of 20 mg lasted for 12–14 hours (see Figure 1).
However, first-generation PPIs do not fully meet the practical needs of clinicians. They are slowly converted into the active form and create the maximum antisecretory effect for eradication only by the fifth to eighth day of therapy. Drugs in this class also include lansoprazole, pantoprazole, rabeprazole and esomeprazole. They bind to the enzymes of the cell wall of parietal cells - H+, K+ -ATPase, and are the most powerful agents that control gastric acid formation.
Using pH-metry, the effect of a new dosage form of Losek MAPS was studied in HP-negative volunteers. After a course of treatment with this drug, the antisecretory effect
in the daytime was even more pronounced than with the use of pantoprazole [9]. However, pharmaceutical companies, which continued to search for new, more effective antisecretory agents, created a new drug - Nexium. The antisecretory effect of Nexium is superior in severity, speed of onset and duration of action to the similar effect of omeprazole in standard doses of 20 and 40 mg, pantoprazole 40 mg and lansoprazole 30 mg [8].
In connection with the above, a new PPI, Pariet (rabeprazole) is of great interest [3]. In the treatment of peptic ulcer and duodenum, it is recommended to take pariet at a dose of 40 mg once a day or 20 mg every 12 hours. The most effective, fast-acting antisecretory and antibacterial drug in eradication regimens is pariet at a dose of 20 mg twice a day. It does not need to be prescribed seven days before starting antibiotic treatment, as is the case with other PPIs, since a reliable antisecretory effect is achieved already on the first day of treatment (from the recommendations of the Russian Gastroenterological Association).
Unfortunately, the presence of HP resistance to antibiotics in some patients is forcing researchers to develop alternative treatment options for patients suffering from H. pylori-associated peptic ulcer disease.
Thus, we have studied the effectiveness of eradication schemes using reserve antibacterial drugs. The best eradication result (90%) was achieved using the regimen: de-nol 240 mg twice a day, 14 days + tetracycline 1 g/day and furazolidone 200 mg twice a day, seven days.
Quite often the question arises about the need for eradication therapy in elderly and senile people. Today, this can be attributed to the fact that with long-term persistence of HP, intestinal metaplasia and atrophy of the gastric mucosa develop, and the risk of developing gastric carcinoma increases. Age-related characteristics of enzymatic activity and atrophic processes in the gastrointestinal tract also change the rate of biotransformation of drugs and disrupt their absorption. It has been noted that the concentration of ranitidine increases in patients over 60 years of age with concomitant pathology of the hepatopancreatobiliary region [1].
The “Achilles heel” of conservative treatment of peptic ulcer disease is, as is known, the high incidence of complications. It has been proven that HP eradication completely prevents complications of peptic ulcer disease. Thus, in the course of four large studies, the course of peptic ulcer disease was studied in patients in whom it manifested itself with bleeding (see Figure 2). As can be seen from the data presented, any other type of treatment does not exclude the danger of recurrent bleeding - within a year after the previous bleeding, it recurs in approximately every third patient. In the case of HP eradication, bleeding does not recur at all (see Figure 2).
| Figure 2. Rate of recurrent bleeding after a course of eradication therapy. |
Evaluation of the effectiveness of eradication is carried out after completion of treatment and is aimed at identifying vegetative and coccal forms of H. pylori. The “Recommendations” clearly define the scheme for carrying out this diagnostic stage:
- timing - no earlier than four to six weeks after the end of the course of anti-Helicobacter therapy, or after treatment of concomitant diseases with any antibiotics or antisecretory agents;
- diagnosis of eradication is carried out using at least two of these diagnostic methods, and using methods that make it possible to directly detect bacteria in biopsy material (bacteriological, histological, urease). It is necessary to study two biopsy specimens from the body of the stomach and one biopsy specimen from the antrum.
The role of antacid drugs in the treatment of peptic ulcer and duodenal ulcer should not be underestimated. These drugs, known since ancient times, reduce the acidity of gastric juice due to chemical interaction with acid in the stomach cavity. Preference is given to non-absorbable antacids - almagel, maalox, phosphalugel, talcid, rutacid. For exacerbation of peptic ulcer and duodenal ulcer, in complex treatment we used rutacid at a dose of 500 mg three times a day + one tablet before bedtime. While taking this remedy, the symptoms of gastric dyspepsia disappeared
by the end of the first or second day of treatment. Despite the introduction into medical practice of modern inhibitors of gastric secretion, antacids remain important as an effective treatment for patients with gastric ulcers and duodenal ulcers.
As a result of treatment, complete clinical and endoscopic remission should be achieved, with negative results of HP testing.
It should be noted that we very rarely encounter cases where a patient has an isolated ulcer. Treatment of combined pathology is associated with a number of problems.
Sometimes conservative therapy is ineffective. This may be due to two factors: the often recurrent course of peptic ulcer disease and the formation of refractory gastroduodenal ulcers. The analysis revealed the reasons for frequent relapses during ulcerative disease, these are HP infection, taking non-steroidal anti-inflammatory drugs, a history of complications of ulcerative ulcer, as well as low compliance. The factors listed above, as well as the latent Zollinger-Ellison syndrome, may be factors contributing to the formation of refractory gastroduodenal ulcers.
In conclusion, we should once again emphasize the extreme importance of developing domestic standards for the treatment of peptic ulcers and duodenal ulcers and their early implementation in the practice of a general practitioner and gastroenterologist. Important arguments in favor of anti-Helicobacter treatment were obtained when assessing the cost/effectiveness ratio. Peptic ulcer is widespread and characterized by a chronic relapsing course. Eradication of H. pylori reduces both direct and indirect costs of ulcerative disease, eliminating the need for expensive maintenance treatment with antisecretory drugs, reducing the risk of repeated exacerbations, complications and, in some cases, surgical treatment.
Thus, modern drug therapy for duodenal ulcers and gastric ulcers can ensure a relapse-free course of these diseases and relieve patients from complications. In most cases, outpatient treatment is sufficient. The success of therapy depends not only on the prescription of the optimal drug combination, but also, to a large extent, on its implementation with the participation of the patient.
Literature.
- Vertkin A.L., Masharova A.A. Treatment of peptic ulcer disease in a modern clinic // Attending physician, October 2000, No. 8. — P. 14-19.
- Grigoriev P. Ya., Yakovenko E. P., Agafonova A. et al. Pyloric helicobacteriosis: diagnosis, treatment // Attending physician, June 2002, No. 6. — P. 3-8.
- Erashchenko P. P., Snegova E. A., Churilin Yu. Yu. Pharmacoeconomic justification for the use of rabeprazole (Pariet) for peptic ulcer // Clinical pharmacology and therapy, 2001, 10 (1). — P. 42-46.
- Ivashkin V. T. Prevention and treatment of chronic diseases of the upper gastrointestinal tract. - M.: "MEDpress - inform", 2002. - P. 127.
- Isakov V. A, Shcherbakov P. L. Comments on the Maastricht Agreement.” — 2, 2000//V International Symposium “Diagnostics and treatment of diseases associated with H. pylori.”, Pediatrics, No. 2, 2002. — P. 5-7.
- Kokueva O.V., Stepanova L.L., Usova O.A. et al. Pharmacotherapy of peptic ulcer disease taking into account concomitant pathology of the gastrointestinal tract // Experimental and practical gastroenterology, 1/2002. — P. 49-52.
- Koltsov P. A., Zadionchenko V. S. Pharmacotherapy of chronic diseases of the digestive system // Practical guide. - M., 2001. - P. 200.
- Lapina T. L., Ivashkin V. T. Modern approaches to the treatment of gastric and duodenal ulcers // Russian Medical Journal. - T. 3, No. 1, 2001. -
- 10-15.
- Lapina T. L. Modern approaches to the treatment of acid-dependent and H. pylori - associated diseases // Clinical perspectives of gastroenterology and hepatology. 1, 2001. —
- 21-27.
- Pimanov S.I. Esophagitis, gastritis, and peptic ulcer - N. Novgorod, 2000. - 376 p.
- Strachunsky L. S., Kozlov S. N. Macrolides in modern clinical practice. - Smolensk, 1998. - 303 p.
I. V. Mayev , Doctor of Medical Sciences, Professor at MGMSU, Moscow
Prevention of peptic ulcers
Stomach ulcers can be avoided if you follow some rules. First of all, give up bad habits, since ethyl alcohol and tobacco reduce the protective properties of the mucous membrane and irritate it.
Diet is no less important in prevention: you need to eat at a certain time, the interval between meals should not exceed 4 hours. You cannot eat dry food, as dry rough food injures the walls of the stomach.
For those who work at night, it is recommended to change jobs to work only during the daytime. It is necessary to avoid stress, treat inflammation of the stomach, hormonal diseases, and visit a gastroenterologist at least once every six months.