“People simply cannot afford to continue to be deprived of microbial diversity, which is already rapidly declining, in part due to antibiotic overuse.”
M. Blazer “When there are not enough microbes”
According to scientists, more than 100 trillion microorganisms, represented by bacteria, fungi, viruses and protozoa, live inside and outside the human body. They form colonies in areas such as the skin, respiratory system, eyes, oral cavity, urogenital and gastrointestinal tract. In each of these areas, microorganisms are organized into communities called the microbiota* or microflora of that area. The composition of the microbiota is individual, almost like fingerprints. It is determined by genetic predisposition and microorganisms received in childhood from the mother and from the environment and can change throughout life under the influence of external and internal factors.
*Microbiota is a community of microorganisms united by a certain area of habitat in the human body, with an established composition and ways of interacting with each other and with the host organism.
For a long time, humanity treated bacteria only as causative agents of dangerous diseases, but over time it came to the understanding that bacteria that permanently reside in the human body not only do not cause harm, but can also be useful to humans. The study of microflora and its connections with various diseases is still ongoing and is one of the most popular topics of scientific research at present.
Why do we need intestinal microflora?
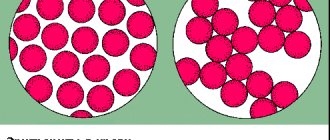
The largest and best studied community of microorganisms is found in the gastrointestinal tract (60-80%), and in particular in the intestines, with a predominance in the colon. The mass of microflora living in the intestines of a healthy person is about 3 kg! The mutually beneficial relationship between the human body and intestinal microflora has been formed over several thousand years under the influence of changes in the environment and diet. It is the state of the intestinal microbiota that most significantly affects the quality and life expectancy of a person.
Microorganisms living in the intestines of a healthy person form normal microflora and are in a state of equilibrium both with the host organism and relative to each other. This ensures the best performance of all its functions by the microbiota.
What functions does intestinal microflora perform?
- Supports the immune system and protects against pathogens.
- Promotes the absorption of nutrients by breaking down and processing fiber.
- Participates in the metabolism of fats, carbohydrates and bile acids, affects the sensitivity of cells to insulin, sugar levels and appetite.
- Synthesizes vitamins K, B1, B12 and essential amino acids necessary for the body.
- Helps maintain the vital activity of intestinal mucosal cells.
- Regulates intestinal motility and the activity of its enzymes.
- Neutralizes toxins: harmful foreign substances and metabolic products.
- Provides optimal permeability of the intestinal wall and reduces the level of inflammation in the body.
During a person’s life, changes can occur in the intestinal microflora under the influence of various factors, which in some cases lead to the development of functional disorders and chronic diseases. Scientific research has confirmed the connection between the state of the intestinal microflora and the development of chronic diseases such as atherosclerosis, cardiovascular diseases, obesity, diabetes mellitus, inflammatory bowel diseases, liver diseases, and malignant neoplasms. Scientists have also discovered that gut microflora can influence brain function and human behavior.
Literature
- Immunostimulating filamentous bacteria: finally tamed!;
- Microflora of the gastrointestinal tract. Propionics website;
- Oleskin A.V. (2009). Neurochemistry, symbiotic microflora and nutrition (biopolitical approach). Gastroenterology of St. Petersburg. 1, 8–16;
- Calm like GABA;
- Dibaise Bäckhed F., Ding H., Wang T., Hooper LV, Koh GY, Nagy A. et al. (2004). The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl. Acad. Sci. USA. 101 (44), 15718–15723;
- Zoo in my stomach;
- Glick-Bauer M. and Yeh M.-C. (2014). The Health advantage of a vegan diet: exploring the gut microbiota connection. Nutrients. 6 (11), 4822–4838;
- Sun J., Qiao Y., Qi C., Jiang W., Xiao H., Shi Y., Le G. W. (2016). High-fat-diet-induced obesity is associated with decreased antiinflammatory Lactobacillus reuteri sensitive to oxidative stress in mouse Peyer's patches. Nutrition. 32 (2), 265–272;
- Ley RE, Bäckhed F, Turnbaugh PJ, Lozupone CA, Knight RD, Gordon JI (2005). Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA. 102, 11070–11075;
- Khan MJ, Gerasimidis K, Edwards CA, Shaikh MG (2016). Role of gut microbiota in the aetiology of obesity: proposed mechanisms and review of the literature. J. Obes. 2016, 7353642;
- Final Report Summary - METAHIT (Metagenomics of the Human Intestinal Tract). European Commission website CORDIS (Community Research and Development Information Service);
- Koeth RA, Levison BS, Culley MK, Buffa JA, Wang Z, Gregory JC et al. (2014). γ-Butyrobetaine is a proatherogenic intermediate in gut microbial metabolism of L-carnitine to TMAO. Cell Metab. 20 (5), 799–812;
- Gut microbiome: the world inside us;
- Korner J. and Leibel R.I. (2003). To eat or not to eat - how the gut talks to the brain. N.Engl. J. Med. 349, 926–928;
- Brugman S, Klatter FA, Visser JT, Wildeboer-Veloo AC, Harmsen HJ, Rozing J, Bos NA (2006). Antibiotic treatment partially protects against type 1 diabetes in the bio-breeding diabetes-prone rat: is the gut flora involved in the development of type 1 diabetes? Diabetologia. 49, 2105–2108;
- Paun A., Yau C., Danska J. S. (2016). Immune recognition and response to the intestinal microbiome in type 1 diabetes. J. Autoimmun. 71, 10–18;
- Costa FR, Françozo MC, de Oliveira GG, Ignacio A, Castoldi A, Zamboni DS et al. (2016). Gut microbiota translocation to the pancreatic lymph nodes triggers NOD2 activation and contributes to T1D onset. J. Exp. Med. 213 (7), 1223–1239.
How to maintain the diversity of intestinal microflora?
Healthy people tend to have a more diverse gut microflora. Therefore, one important aspect of health is microbial diversity in the gut.
Tips to help preserve intestinal microflora:
- eat a variety of foods and include vegetables and fruits, whole grains rich in fiber, and dairy products in your diet;
- maintain a healthy weight;
- normalize night sleep;
- engage in physical activity;
- stop smoking and drinking alcohol.
- do not take antibiotics and other medications that affect microflora, including food supplements with prebiotics and probiotics, without a doctor’s prescription;
The diet, and especially the presence or absence of a sufficient amount of indigestible plant fiber, has a significant impact on the composition of the intestinal microflora. To choose a suitable diet, you can use the rule of three “Ps”: including in your daily diet foods that naturally contain polyphenols* and prebiotics* from plant foods and probiotics* from naturally fermented dairy and plant products. This diet corresponds to the Mediterranean diet.
*Polyphenols are organic compounds found in most plants and have antioxidant properties.
*Prebiotics are food components that can only be digested with the help of enzymes secreted by intestinal microflora bacteria and serve for their nutrition and growth. Prebiotics are found naturally in food and can be isolated and formulated as food supplements; there are also artificially synthesized prebiotics.
*Probiotics are live microorganisms that are part of the normal intestinal microflora, improve the condition of the gastrointestinal tract (GIT) when used correctly and can be found both naturally in food and in the form of dietary supplements.
List of foods rich in probiotics:
- natural yogurt with active live culture without added sugar. Not all yogurts contain live probiotics; the composition of the product is indicated on the label;
- other fermented milk products - kefir, yogurt, acidophilus, bififruit;
- unpasteurized sauerkraut;
- fermented soy products (tempeh, miso paste, natto);
- kimchi - a Korean dish made from pickled vegetables;
- unpasteurized vegetable pickles prepared without vinegar;
- some types of cheese (mozzarella, gouda, cheddar).
Types of prebiotics and products that contain them:
- oligosaccharides, carbohydrates consisting of simple sugars, are found in dairy products, fresh fruits and vegetables;
- polysaccharides are complex carbohydrates, found mainly in tubers and root vegetables (inulin) and in many vegetables, fruits, grains and legumes (cellulose, pectin).
Is there an alternative to antibiotics?
The vast majority of antibiotics used in medicine . They have become so firmly established in everyday life that many doctors, out of habit, prescribe them even for minor reasons (say, for a simple cold). And people who are accustomed to trusting people in white coats regularly follow all the recommendations. With all the ensuing consequences that are described above. However, it is encouraging that recently there has been a tendency to abandon the use of synthetic antibiotics “for all occasions.” Today there is an understanding that if, in the treatment of a particular disease, an artificial antibiotic is not a mandatory drug and, in principle, one can do without its use, then it is better to turn to an alternative - antibiotics of plant origin. Moreover, the medicinal properties of plants have been known for a very long time.
Many of them - for example, elecampane, licorice and bearberry - contain glycosides. Many of these organic compounds (they are also called theol glycosides or phytoncides) are similar in their action to antibiotics . Their use has proven effective in the fight against harmful microorganisms, but there are no side effects, not to mention addiction and complications. Experts recommend: if treating your disease in an acute form is impossible without synthetic antibiotics, then use natural antibiotics for its chronic course. Having, of course, agreed on this issue with your doctor, because medications should also not be taken uncontrolled. In addition to the above-mentioned plants, onions and garlic, horseradish and cranberries, apples, citrus fruits and dogwoods . Garlic also contains the substance allin. Interacting with food enzymes, it turns into allicin, which is known for its pronounced bactericidal properties.
Pathogenic microorganisms do not feel very comfortable in the vicinity of phytoalexins - substances that are a type of phytoncides . Their amazingness is that at first they are simply absent from plants. But as soon as pathogenic microbes appear “on the horizon,” the process of their synthesis immediately begins. Phytoalexins can be formed in potatoes, carrots, peppers and a number of other vegetable crops.
Another effective alternative to artificial antibiotics is called bacteriophages . They have not yet found widespread use, but in medical circles they are sure that everything is moving towards this. Bacteriophages are some types of viruses that have a selective effect on certain bacteria. That is, when they treat specific diseases, only causative microorganisms will be destroyed. Since each illness has its own bacteriophage, there is no need to fear damage to beneficial intestinal microflora. Bacteriophages, unlike conventional antibiotics, do not have any effect on internal processes in the body and certainly do not disrupt their course. But there are also disadvantages: it is difficult to select “their” viruses for certain pathogenic bacteria. And treatment with bacteriophages usually takes longer than a traditional course of antibiotics. But both doctors and patients are inclined to believe that these disadvantages can be easily accepted and lived with. The main thing is that bacteriophages do not cause damage to the human body, which is already weakened due to the underlying disease.
Modern ideas about intestinal dysbiosis (dysbacteriosis)
Dysbiosis (dysbacteriosis) is a pathological condition in which the qualitative and quantitative composition of the intestinal microflora is disrupted compared to normal. For the colon, this term refers to a decrease in the number of beneficial microorganisms and an increase in the number of representatives of pathogenic flora. For the small intestine, in which in a healthy state the number of microorganisms is minimal, dysbiosis, on the contrary, is associated with an increase in the number of microorganisms. Small intestinal dysbiosis is called bacterial overgrowth syndrome (SIBO).
Causes of dysbiosis (dysbiosis) of the colon:
- unbalanced diet and insufficient fiber intake;
- water quality;
- alcohol abuse and smoking;
- antibacterial therapy and occupational exposure to antibiotics;
- long-term use of other medications;
- any acute and chronic infections;
- developmental anomalies, operations and their complications;
- primary and secondary immunodeficiencies;
- chronic gastrointestinal diseases and endocrine disorders;
- radiation;
- elderly age.
At the initial stage, colon dysbiosis has no noticeable symptoms and is reflected only in laboratory examination of stool samples. At a more advanced stage, noticeable manifestations appear.
Symptoms and manifestations of colon dysbiosis:
- bowel dysfunction - constipation or diarrhea;
- bloating and increased gas formation;
- stomach ache;
- food or drug allergies;
- metabolic disease;
- anemia, abnormal cholesterol levels;
- functional intestinal disorders;
- liver damage and others.
How to restore intestinal microflora?
In healthy people in the absence of chronic diseases, the microflora is restored independently and does not require any additional measures.
The need for its correction may arise after suffering from acute gastrointestinal diseases and taking medications that affect the composition of the microflora due to flatulence, constipation, diarrhea, abdominal pain and food allergies.
Correction of the composition of microflora in the colon requires preliminary diagnosis and an integrated approach to treatment. Restoring the composition of intestinal microflora includes several stages:
- Treatment of the underlying disease that caused dysbiosis.
- Liberation of the gastrointestinal tract from pathogenic pathogens and their toxins.
- Correction of nutrition with the addition of foods that promote recovery.
- Restoration of impaired intestinal functions and the composition of the microflora itself using pre- and probiotics or synbiotics.
*Synbiotics are natural products or complex nutritional supplements with a combination of prebiotics and probiotics.
To date, the only scientifically proven means that can deliver microorganisms to the intestines to restore intestinal microflora is fecal transplantation.
Pre and probiotics are currently used as a means of promoting self-healing of the colon microflora. Their effect is not to add beneficial bacteria to the microflora, but to suppress pathogenic microorganisms, reduce the level of inflammation in the intestines and trigger the renewal of the intestinal microflora. There are scientific studies that confirm the improvement in well-being when taking such drugs.
If symptoms similar to those of dysbiosis appear, we recommend that you consult a gastroenterologist for examination and treatment. You can undergo the necessary examinations and get advice from specialists at the Gastroenterological Department. We also have a comprehensive “Check-up Intestinal Examination” at a special price, which includes all the necessary examinations and consultation with a gastroenterologist.
Probiotics are the best protection for microflora
Normoflorins L, B, D
How can we normalize the intestinal microflora that has become a victim of traditional antibiotic therapy? This question is more than relevant today for a large number of people, but there is only one answer - only probiotics . This is the name for special products that can not only support and restore normal intestinal microflora, but also populate the intestines with such microflora. The uniqueness and advantage of probiotics is that they contain live strains of beneficial bacteria. When they colonize the intestines, the opportunistic flora is forced to give up their positions. As a result, the digestive system is restored to its healthy state prior to the course of antibiotics.
In addition to restoring normal intestinal function and improving digestion, probiotics participate in strengthening local and general immunity, and synthesize much-needed vitamins such as groups B and K. All these vital processes occur thanks to the active work of lacto- and bifidobacteria, which are part of probiotic complexes. To forestall your possible doubts, we note: the use of probiotics as a restorative agent after antibiotic therapy is absolutely safe. As for the effectiveness, it can be judged by the example of biocomplexes known as Normoflorins . These are special natural preparations, produced in liquid form, which are a mixture of lactobacilli and bifidobacteria with their metabolic products - vitamins and minerals, antimicrobial nutrients and organic acids. In addition, Normoflorins contain a very valuable ingredient - the disaccharide lactitol, which serves as excellent nutrition for a person’s own microflora, thereby stimulating its growth and development.
The first Russian scientist to seriously study the effect of probiotics on the restoration of microflora was I.I. Mechnikov. He based his work on observations of lactic acid bacillus, arriving at excellent results. However, probiotics are not necessarily just bacteria. These may include other protozoa. Let's say yeast.
Sources
- Yu.V. Yudina, Doctor of Medical Sciences, Prof. A.A. Korsunsky, Doctor of Medical Sciences, Prof. A.I. A minova, G.D. Abdullaeva, Doctor of Medical Sciences, Prof. A.P. Prodeus “Intestinal microbiota as a separate system of the body”, Evidence-based gastroenterology, 2021, T. 8, No. 4-5, p. 36-43.
- Zimmerman Ya.S. Gastroenterology: a guide. – 2nd ed., revised. and additional – M.: GEOTAR-Media, 2015. – 816 p.: ill.
- T.Yu. Demidova, K.G. Lobanova, O.Sh. Oinotkinova “Intestinal microbiota as a risk factor for the development of obesity and type 2 diabetes mellitus,” Therapeutic archive, 10, 2021.
- Monograph edited by E.L. Nikonova and E.N. Popova "MICROBIOTA".