Zollinger-Ellison syndrome - what is it?
This pathology is a clinical manifestation of gastrinoma, which is a hormonally active tumor.
A number of tumor variants develop aggressively with the formation of metastases. The tumor produces an excessive amount of gastrin, thereby forcing the gastric mucosa to respond to this by producing a large amount of secretion, which causes ulcers, vomiting, and diarrhea. In some cases, the pathology develops so rapidly that the need for surgery arises in less than a day.
In the 50s of the 20th century, the pathology was considered a gastric ulcer, which occurs with diarrhea. There was also excessive production of juice by the stomach, as well as a high level of gastrin in the blood.
The cause of the pathology was considered:
- Serious eating disorders;
- Excessive alcohol consumption;
- Stress.
Only then did they find out that the pathology was initiated by a tumor of a neuroendocrine nature, which, as a rule, is localized in the gastrointestinal tract.
The described syndrome is a rather rare pathology, found in 1 person in 1,000,000. Even in those who suffer from stomach ulcers, the pathology occurs in about 1%.
Most people susceptible to pathology are men 40-55 years old.
Causes of pathology
Tumor cells produce the hormonal substance gastrin, which, in turn, provokes the stomach to produce hydrochloric acid in excessive quantities.
Almost 80% of tumor cases occur in the duodenum, the rest are localized in the pancreas.
The cause of the tumor is a genetic mutation.
Neoplasia of the gastrin-producing type can also be localized in other organs, for example, in the lungs, and their manifestations can be a described pathology.
Ménétrier's disease
Ménétrier described two types of disorders associated with polypoid growths in the stomach, which he tried to associate with gastric carcinoma [10].
- The first (called “polyadenomes polypeux”) consists of multiple non-confluent gastric polyps, which are currently classified as hyperplastic polyps [11].
- The second (which he called Ménétrier's polyadenomatosis, or multiple sheet-like adenomas) is a new type associated with foveal hyperplasia and should by law bear his name [8].
Who is at particular risk?
It is difficult to predict the development of pathology. However, by studying nepotism, one can assume its genetic roots even in cases where the symptoms were subtle or were mistaken for the manifestation of other diseases. The pathology of the hereditary form is in most cases localized in the duodenum.
If we talk about those who were affected by the pathology by accident, then it is necessary to note its localization in the pancreas.
Hereditary neoplasms can develop as multiple tumors. The pathology is milder and oncological gastrinoma is less common. However, surgical intervention does not provide a complete cure for this form.
Diagnosis and course of gastrinoma
To diagnose Zollinger-Ellison Syndrome, a gastrin test is performed. A concentration of 1000 ng per liter may indicate the presence of a disease. If chromogranin is confirmed in the serum, everything indicates the presence of a neuroendocrine tumor. Treatment-resistant abdominal pain of atypical localization confirms the diagnosis.
To confirm the location of the tumor, it is important to undergo a series of studies. For this purpose, visualization diagnostics are carried out:
- Octreotide scan;
- PET-CT;
- MRI;
- CT scan.
When to see a doctor
Abdominal pain, swelling, ulcers or changes in body shape, as well as gastrointestinal disorders, diarrhea may be symptoms of the disease and therefore it is necessary to consult a specialist without waiting for such manifestations to worsen.
In addition, you need to undergo an examination if you have noted:
- digestive disorders;
- heartburn;
- inflammation of the larynx;
- weight loss;
- constant pressing pain;
- irritability;
- fatigue;
- loss of appetite.
Symptomatic manifestations
Pathology can manifest itself in various manifestations:
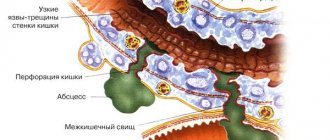
- Ulcers of the stomach and duodenum;
- Constant intense pain in the upper abdomen;
- Copious, semi-formed or watery stools;
- Prolonged heartburn and belching;
- Narrowing of the esophagus;
- Gastrointestinal bleeding, etc.
With the oncological nature of the pathology, a decrease in the patient’s weight is observed, and a significant decrease.
Superior vena cava syndrome (SVVC)
Symptoms of the disease
SZE causes severe abdominal pain, which usually has an atypical localization. Patients often suffer from reflux, in which stomach contents back up into the esophagus. Stomach acid causes inflammation of the mucous membranes and heartburn. A common consequence of reflux is inflammation of the larynx. Half of the patients suffer from diarrhea.
All this leads to loss of electrolytes and vitamins. Some patients experience vomiting of blood.
In addition, speaking about the symptoms of Zollinger-Ellison Syndrome , it should be noted that an excess of gastric juice inactivates lipases. Since these enzymes support digestion, the absorption of fats in the small intestine is disrupted, and they enter the large intestine, resulting in fatty changes in the consistency of stool. Sometimes the pH level in the blood increases. In rare cases, the production of parathyroid hormones increases.
Diagnostic measures
The presence of pathology can be determined by observing a multiple increase in the level of gastrin in the blood.
When performing an endoscopic ultrasound examination, you can see the tumor, but only part of it, because it is located in the wall of the duodenum.
Computed tomography and magnetic resonance imaging examinations are clearer in terms of sensitivity. The degree of this sensitivity determines the size of the tumor. In any case, it must be detected for further monitoring of development.
The effectiveness of angiography and PET is associated with a good blood supply to the tumor. The final diagnosis is announced after examination of the biopsy specimen.
As practice shows, 2/3 of tumors are not malignant; therefore, there are no metastases. Sporadic tumors are aggressive, but this is not typical for multiple endocrine neoplasia.
Pancreatic cancers usually metastasize. They can cause damage to the liver and lymph nodes of the peritoneal cavity.
Tumors of the duodenum most often affect bones, usually flat ones.
The possibility of metastases depends on the size of the tumor focus; they can cause increased pathology.
Introduction
Currently, the concept of “diseases associated with increased secretion of hydrochloric acid” has become widespread. It describes a spectrum of pathological conditions in which increased production of hydrochloric acid by the gastric mucosa is one of the main causes of patient complaints [8]. The fact that hydrochloric acid is the main component of gastric juice has been known for a long time and was established by William Prout (1785-1850) in 1823 [28]. Paracelsus (1493-1541), contrary to the then dominant according to the Holy Church, assigned a significant role to acid in digestion [28].In accordance with modern ideas about the pathogenesis of diseases associated with increased secretion of hydrochloric acid, the most important is the imbalance between acid-peptic aggression and the protective mechanisms of the mucous membrane of the gastrointestinal tract [60 ] Acid overproduction is important, but, as a rule, not the only cause of the development of symptoms of the disease [41].The concept of “diseases associated with increased secretion of hydrochloric acid” defines the circle of patients for whom it is advisable to prescribe therapy aimed at reducing acid production [8].
Modern principles of treatment of diseases associated with increased secretion of hydrochloric acid are based on the prescription of proton pump inhibitors (PPIs) in the first line of complex therapy. The World Congress of Gastroenterology, held in Rome in 1988, recognized PPIs as the main group of acid-controlling drugs [57]. Significant advances in the clinical use of antisecretory drugs have made adjustments to surgical gastroenterology. The number of operations for peptic ulcer disease has decreased significantly. In 1993, at a conference of gastroenterologists at Yale, it was agreed that vagotomy could no longer be considered as a method of choice in the treatment of peptic ulcer disease [57].
Currently, PPIs are used to treat a wide range of gastrointestinal diseases. First of all, we are talking about chronic gastritis, duodenitis and peptic ulcers of the stomach and duodenum, including for the prevention of the development of acute ulcers of the stomach and duodenum with long-term use of non-selective NSAIDs, combination therapy with antibiotics for the eradication of Helicobacter pylori,
as well as gastroesophageal reflux disease and Barrett's esophagus. The principles of treatment of these diseases are sufficiently covered in the literature [4, 5, 7, 11, 17, 18, 23, 24, 32, 38-40, 42, 44, 45, 49] and published in the standards of medical care approved by the Ministry of Health and Social Development of Russia. It should be noted that PPI therapy can mask the symptoms of malignant diseases and before starting treatment it is necessary to verify the diagnosis and also exclude the presence of a malignant tumor of the gastrointestinal tract in the patient.
In modern literature, unreasonably little attention is paid to the role of PPIs in the treatment of Zollinger-Ellison syndrome, in which increased production of hydrochloric acid plays a key role in the development of symptoms of the disease, and antisecretory therapy has a number of features.
General information about Zollinger-Ellison syndrome
Zollinger-Ellison syndrome is characterized by the development of peptic ulcers of the duodenum and stomach, difficult to treat, prone to gastrointestinal bleeding and accompanied by diarrhea, against the background of gastrin-producing neuroendocrine neoplasia (gastrinoma). The combination of neuroendocrine neoplasia of the pancreas with an extremely aggressive course of peptic ulcer disease was described by American surgeons R. Zollinger and E. Ellison in 1955 [54], and in the world literature a complex of clinical manifestations of ulcerogenic adenoma (gastrinoma) bears their names.
The incidence of Zollinger-Ellison syndrome is 0.5-3 cases per 1 million population per year [12, 35, 43]. In most cases (50-88%), gastrinomas are localized in the duodenum. However, these neoplasms can occur in the stomach, liver, common bile duct, ovary, and also outside the abdominal cavity (in the heart, lung) [15, 51, 52]. The duration of the disease before verification of the diagnosis averages 5.2 years, the symptoms of the disease correspond to hypersecretion of hydrochloric acid: the development of peptic ulcers or gastroesophageal reflux disease against the background of diarrhea [12]. Abdominal pain, usually associated with peptic ulcer or gastroesophageal reflux disease, is observed in 75-98% of patients, diarrhea occurs in 30-73% of cases, heartburn in 44-56%, gastrointestinal bleeding in 44-75%, nausea/vomiting - in 12-30%, weight loss - in 7-53% of cases [36]. Presence of H. pylori
with peptic ulcer disease in patients with Zollinger-Ellison syndrome is observed in 24-48% of cases, while in patients with idiopathic peptic ulcer disease - in more than 90%. The absence of Helicobacter pylori infection in a patient with recurrent severe peptic ulcer disease should alert the clinician to the presence of Zollinger-Ellison syndrome [51]. In patients with multiple endocrine neoplasia syndrome type 1 (MEN-1), clinical manifestations of Zollinger-Ellison syndrome (20-30% of patients with MEN-1) occur at an earlier age, on average at 32-35 years [37].
More than 98% of patients with Zollinger-Ellison syndrome have an increased level of fasting serum gastrin, 87-90% of patients have increased secretion of hydrochloric acid in the stomach, and 100% of patients have a pH level of gastric juice that does not exceed 2.0 [35, 36 ]. Hypergastrinemia usually exceeds 1000 pg/ml, while in peptic ulcers the blood gastrin level rarely exceeds 100 pg/ml. Acid production in patients with Zollinger-Ellison syndrome exceeds 100 mmol/h.
The size of gastrinomas localized in the duodenum in 77% of patients does not exceed 1 cm, while the size of gastrinomas detected in the pancreas averages 3.8 cm; only 6% of patients have pancreatic gastrinomas with a diameter of less than 1 cm Similar to other neuroendocrine neoplasias of the gastrointestinal tract, gastrinomas are classified according to the WHO (2010) and TNM systems [6] and in most cases are characterized as G1-G2 neuroendocrine tumors. At the time of diagnosis, they have signs of invasive growth and metastases to the lymph nodes [3, 20, 21]. Metastases to the liver are most typical for pancreatic gastrinomas and are detected in 22-35% of such cases. Distant metastases of duodenal gastrinomas are found in no more than 10% of patients [16, 20, 21]. Histologically, most gastrin-producing neoplasias have a trabecular structure, are highly differentiated, and the Ki67 proliferation index is often about 2% and rarely exceeds 10% [16, 20, 21].
The main treatment method for patients with gastrin-producing neuroendocrine neoplasia with Zollinger-Ellison syndrome is surgery [19]. The five-year survival rate of patients with sporadic gastrinomas reaches 45% [16, 29-31]. The question of the need for surgical treatment of patients with gastrin-producing neuroendocrine neoplasia in the framework of MEN-1 remains controversial [2, 48]. There is an opinion that it is advisable to perform surgical intervention in such patients only if the size of neoplasia is more than 2 cm. This position is associated with a low probability of cure and good survival rates for patients with small tumors (up to 2 cm) against the background of symptomatic PPI therapy [29]. According to other authors, surgical treatment is indicated for all patients with Zollinger-Ellison syndrome as part of Wermer syndrome [1, 2, 47].
Mechanism of action of proton pump inhibitors
One of the PPIs widely used in clinical practice is Controloc, which is effective in the complex treatment of gastrointestinal diseases associated with increased secretion of hydrochloric acid [7]. The drug molecules, accumulating in the intracellular tubules of parietal cells, are transformed into tetracyclic sulfenamide, which is covalently incorporated into the cysteine groups of H+/K+-ATPase, thereby making the enzyme unable to participate in the process of ion transport. Thus, the drug suppresses the final phase of hydrochloric acid formation. To restore the ability to secrete hydrochloric acid, the parietal cell is forced in such cases to synthesize a new enzyme molecule [58].
Controloc is rapidly absorbed, its maximum concentration in the blood plasma is achieved even after taking one dose of the drug. On average, maximum concentrations of 1.0-1.5 mcg/ml are achieved 2.0-2.5 hours after dosing; these levels remain constant after repeated dosing. Controloc differs from omeprazole and lansoprazole in the structure of radicals on the pyridine and benzimidazole rings, which makes it more stable at pH values close to neutral [13, 33]. The volume of distribution is 0.15 l/kg, the clearance of Controloc is approximately 0.1 L/h/kg, and the half-life is 1 hour. Due to the specific activation of Controloc in parietal cells, the half-life does not correlate with the duration of action (inhibition of acid secretion). Pharmacokinetics does not change after single or multiple doses. In the dose range from 10 to 80 mg, the pharmacokinetics of the drug remains linear both after oral administration and after intravenous administration. Plasma protein binding is 98%.
The drug is metabolized in the liver. The main route of excretion of metabolites is renal (80%), 20% is excreted in feces. Controloc is completely absorbed after oral administration. The absolute bioavailability of the drug in the form of tablets resistant to gastric juice is 77%. Eating food does not affect the maximum concentration of the drug and its bioavailability. Patients with impaired renal function (including those on hemodialysis) do not need to reduce the dose of Controloc. As in healthy subjects, the half-life of the drug in these patients is short. In patients with liver cirrhosis (class A and B), the half-life of the drug increases to 3-6 hours and its maximum concentration in the blood plasma increases by 1.3 times compared to that in healthy people. In patients with severe liver dysfunction, the daily dose should be reduced to 20 mg. A slight increase in maximum concentration in elderly patients compared to the corresponding data in younger patients is not clinically significant [46, 50].
It is known that racial genetic characteristics can influence the severity of inhibition of acid formation [56]. Metabolism of Controloc occurs in the liver with the participation of cytochrome P450 isoforms: CYP2C9, CYP2C19, CYP2D6 and CYP3A4. Polymorphism of the gene encoding the CYP2C19 isoform determines different rates of PPI metabolism. There was a significant variation in the individual duration of the antisecretory effect from 1 to 12 days [14, 55]. Therefore, in order to avoid “failures” during PPI therapy, the selection of drugs should be carried out under the control of 24-hour pH measurements [59].
Features of the use of Controloc for Zollinger-Ellison syndrome
The symptomatic treatment of patients with Zollinger-Ellison syndrome has changed dramatically with the introduction of PPIs into clinical practice [10]. It is currently recommended to refrain from gastrectomy, performed to prevent the development of acute ulcers [53], especially if surgical treatment for gastrin is radical [19]. A decrease in acid production when using standard therapeutic doses of PPIs for the treatment of peptic ulcers helps to reduce the intensity of symptoms of the disease in almost all patients with Zollinger-Ellison syndrome. The use of H2 blockers in therapeutic doses, as a rule, does not provide such a significant clinical effect [9, 51].
A number of studies have been published proving the effectiveness of Controloc in the symptomatic treatment of Zollinger-Ellison syndrome [10, 22, 25-27, 34]. When taken orally, a rational daily dose of Controloc in such patients is considered to be 120 mg. The selection of the dose of the drug must be individual. The daily dose can range from 40 to 160 mg [10]. Intravenous administration of Controloc is also effective; in 93% of patients with Zollinger-Ellison syndrome, intravenous administration of 80 mg per day is adequate and is not accompanied by serious adverse events [22, 26]. Controloc is also effective for long-term maintenance therapy of Zollinger-Ellison syndrome. In most patients, control over the symptoms of the disease was achieved by taking 40-80 mg of the drug per day (see figure)
[25].
Figure 1. Dynamics of average acid production in patients with Zollinger-Ellison syndrome during long-term use of various daily doses of Controloc [25].
Long-term use of PPIs is associated with two other aspects. Firstly, their uncontrolled long-term use has led to an increase in the number of patients with advanced gastrinomas. Symptoms of the disease are masked by effective suppression of acid production, which is why multiple ulcers or ulcers with uncharacteristic localization are becoming less common [51]. Secondly, it should be remembered that long-term use of PPIs leads to hypergastrinemia in patients with peptic ulcer disease without Zollinger-Ellison syndrome [32]. In this regard, it is necessary to temporarily stop taking medications before examining gastrin levels. In itself, an increase in gastrin levels is not enough to verify Zollinger-Ellison syndrome. The causes of hypergastrinemia can be hypo- and achlorhydria (with chronic atrophic gastritis, pernicious anemia), as well as H. pylori infection,
gastric outlet stenosis, renal failure, short small bowel syndrome.
Thus, Controloc is an effective and safe treatment for a number of diseases associated with increased secretion of hydrochloric acid. The principles of treatment for these diseases are determined by the standards of medical care approved by the Ministry of Health and Social Development of Russia. There are features of the use of PPIs in the symptomatic treatment of patients with Zollinger-Ellison syndrome that are not sufficiently covered in the literature; there are no Russian standards for the treatment of such patients. When prescribing Controloc to patients with Zollinger-Ellison syndrome, it is recommended to increase its daily dose to 120 mg when administered orally and to 80 mg when administered intravenously. It is advisable to monitor blood gastrin concentrations in patients receiving control for a long time only after the drug has been discontinued in advance. Otherwise, detected hypergastrinemia will have no diagnostic value. Prolonged use of Controloc in this group of patients is also effective.
Treatment
A radical method of treating pathology is tumor removal. In this case, fiber-optic diaphanoscopy of the duodenum and lateral duodenotomy are performed. As a rule, metastases are detected at the time of surgery, which means that only 30% of patients can achieve a complete cure.
The effectiveness of removing a significant part of the stomach is low: the risk of rapid recurrence is quite high.
Several decades ago, the method of total gastrectomy was widely used. Now they resort to it if conservative treatment does not give positive results and the course of the ulcer is complicated.
For therapy, drugs that reduce the level of hydrochloric acid are used. Their use may be indicated for life, since the risk of relapse is high. The doses of drugs exceed the usual ones prescribed for a standard ulcer.
In case of oncology and it is impossible to perform surgery on the tumor, chemotherapy is used.
Pathogenesis
The pathogenesis of Ménétrier's disease is not entirely understood, but may be mediated by transforming growth factor alpha (TGF-alpha). TGF-alpha increases gastric mucus production and inhibits acid secretion [12-14]. The level of TGF-alpha in the cells of the gastric mucosa in patients with Ménétrier's disease is significantly increased [12]. The role of TGF-alpha is further supported by a mouse study in which overproduction of TGF-alpha is associated with significant hyperplasia of gastric mucus-producing cells comparable to that found in humans with Ménétrier's disease [12]. These mice also had reduced basal and histamine-stimulated acid secretion, similar to that observed in humans with Ménétrier's disease [12,13,15]. TGF-alpha may exert its effect by binding to epidermal growth factor receptors. This was suggested based on a report of a patient who experienced clinical improvement after treatment with monoclonal antibodies directed against epidermal growth factor receptors [16]. A similar connection with cytomegolovirus infection is observed in the so-called childhood Ménétrier's disease. Its mechanism can also be realized through TGF-alpha [17]. However, during various types of inflammation and regenerative responses in the stomach, increases in foveal TGF-alpha may also be observed, demonstrating that these findings may be nonspecific [18]. In addition, this pathology may be an example of the incorrect use of the term Ménétrier's disease to other forms of hypertrophic gastropathy.
Diagnosis
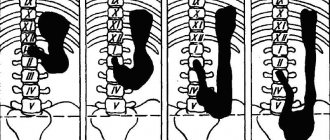
The diagnosis of Ménétrier's disease is based on the identification of extreme foveal hyperplasia with glandular atrophy on biopsy in a patient with significant enlargement of the gastric folds observed on endoscopic examination or barium radiography. A full-thickness or loop biopsy is usually necessary [3,22]. Enlarged folds are limited to the body and fundus of the stomach. The folds are usually symmetrically enlarged, although asymmetrical "polypoid" enlargement may rarely occur.