An irreversible phenomenon during which cells, tissues, and organs cease their vital activity is called necrosis. It can be triggered by pathogenic microbes, mechanical, thermal, chemical, infectious and toxic agents that contribute to tissue destruction. In addition, necrosis can occur as a result of allergies or impaired blood circulation. Taking into account the state of the body and unfavorable local factors, it is possible to determine the pronounced degree of cell necrosis.
The provoking factors for the occurrence of necrosis are pathogenic microorganisms, fungi, and viruses. If blood circulation is impaired and there is hypothermia in this part of the body, vascular spasm will increase and severe disruption of blood circulation will occur. With excessive overheating, metabolism increases, and if blood circulation is impaired, the risk of developing a necrotic process increases.
How does necrosis manifest itself?
If we talk about the first symptoms of necrosis, they are presented in the form of numbness and lack of sensitivity. In such a situation, you must immediately visit an experienced and qualified doctor at a medical center. In addition, the skin becomes pale. This happens because blood circulation is impaired. Over time, the skin will acquire a bluish tint, then turn black or dark green. In the presence of necrosis in the lower extremity, a person notices rapid fatigue while walking, a feeling of coldness, cramps appear, as well as lameness, as a result of which non-healing trophic ulcers will form, which will necrotize over time.
Due to the fact that the respiratory and central nervous systems, kidneys, and liver cease to function normally, blood circulation is disrupted, and a person’s general condition of the entire body deteriorates. In addition, the immune system decreases, as concomitant blood diseases, anemia appear, and metabolic processes are disrupted, the body is depleted, hypovitaminosis and fatigue are observed.
Symptoms
The first signs of dry gangrene are decreased sensitivity in the area of necrosis. If an arm or leg is affected, the complaints are often related to the fact that the limb is always cold, regardless of the air temperature. Motor functions deteriorate, the skin becomes dry, hair stops growing on it, ulcers and wounds appear that do not heal for a long time.
Other symptoms:
- pain in the tissues located just under the layer of skin, which goes away only after the nerve cells die,
- tightness and dryness of the skin,
- brittle and dry nails,
- appearance of the skin marbling effect,
- fungal infection of the skin and nails,
- cramps in the toes and calf muscles at night,
- change in skin color to black or dark brown (Fig. 2),
- absence of unpleasant odor at the site of necrosis,
- gradual increase in the affected area.
Figure 2. Dry gangrene of the left foot.
Source: Journal of cutaneous and aesthetic surgery / Open-i (NonCommercial-ShareAlike 3.0 Unported (CC BY-NC-SA 3.0) With dry gangrene, a person feels quite well and has no symptoms of intoxication. The affected tissue gradually dries out and mummifies, sometimes it can be detached from the body along the dividing line without any intervention, and this result is considered equal to a cure.
Important! As a rule, dry gangrene does not develop into other forms of necrosis - wet or gas gangrene. Rarely, it can cause sepsis or septic shock if tissue breakdown products enter the bloodstream. In this case, the patient’s condition sharply worsens (body temperature rises or falls, chills occur, blood pressure decreases) and often threatens death.
Varieties
Given the changes that occur in the tissue, there are some forms of necrosis. Namely:
- The cause of coagulation or dry necrosis is the folding, compaction, drying of tissue protein, which then becomes a curdled mass. This is the result of the fact that blood has stopped flowing and moisture has evaporated. Areas of tissue become dry, brittle, and also acquire a dark brown or yellowish gray tint with clear demarcation lines. In the place where the dead tissue was rejected, ulcers will appear, a purulent process will develop, and an abscess will form. The localization of dry necrosis is the spleen, kidneys, and umbilical cord stump in a newborn child.
- With colliculative or wet necrosis, swelling, softening and liquefaction of dead tissue occurs, and a mass with a gray tint is formed and a putrid odor appears.
There are some types of necrosis
1. If the blood supply to a tissue or organ suddenly stops, a heart attack occurs. The term ischemic necrosis refers to the death of any part of a vital organ (brain, heart, intestines, lungs, kidneys, spleen). If the infarction is small, autolytic melting or resorption is observed, followed by tissue restoration. A heart attack can result in impaired tissue functioning, various complications, and even death.
2. If necrosis of a section of bone tissue occurs, the localization of which is the sequestral cavity, this is called sequestration. In such a situation, this area will separate from healthy tissue. The reason for this is a purulent process.
3. Death of the skin, mucous surface, and muscle tissue is called gangrene. The cause of gangrene is tissue necrosis.
4. The presence of bedsores is observed in a person who is completely immobilized. This is explained by prolonged compression of the tissue and damage to the skin. As a result, deep purulent ulcers form.
Causes
Dry gangrene develops under the influence of various negative factors that provoke tissue destruction and rejection.
Main reasons:
exposure to very high or low temperatures – burns or frostbite,
- electric shock: necrosis often occurs in burned tissues and at the points of entry and exit of electrical discharge,
- burns caused by caustic chemicals (alkalis or acids), under the influence of which coagulation (denaturation) of cellular protein occurs,
- problems with blood circulation in certain systemic pathologies, for example, diabetes or atherosclerosis,
- thrombosis or vascular damage due to trauma in patients with underweight and asthenia.
Dry gangrene usually develops in thin people whose tissues lack moisture. In obese patients, wet gangrene often begins, since any liquid is a breeding ground for the proliferation of pathogenic microflora.
Necrosis develops under the influence of a number of predisposing factors of different nature:
- Individual anatomical and physiological characteristics of a person
- a history of infectious diseases,
- alcohol poisoning or prolonged exposure to toxic substances,
- metabolic problems
- low hemoglobin level,
- prolonged fasting or exposure to low temperatures,
- dehydration,
- diseases of the cardiovascular system,
- congenital vascular pathologies.
- Local factors
- narrowing of the lumen of blood vessels due to cholesterol deposits,
- compression of a vessel by a hematoma in nearby tissues,
- vascular anastomosis.
- External factors
- vascular spasm, for example, due to sudden cooling,
- exposure to radiation,
- accelerating metabolism in damaged tissues by applying hot compresses or taking hot baths against the background of anemia.
Smoking, constant wearing of tight shoes, and low immunity can also lead to poor circulation.
Electric shock can cause tissue damage. Photo: focuspocusltd / Depositphotos
Stages of the disease
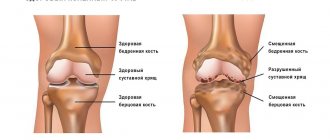
There are several stages of development of this disease. The first stage is characterized by a slight change in bone tissue, when the hip joint maintains functionality, and painful sensations are periodic. At the second stage, cracks begin to form on the surface of the joint, its mobility is impaired, and the person experiences constant pain. The third stage is called secondary arthrosis, when the acetabulum is involved in the process. There is a significant decrease in joint mobility. This stage is manifested by constant and severe pain. At the fourth stage, the bone begins to deteriorate, the muscles atrophy, and the pain is not eliminated by medications.
What is aseptic necrosis of the femoral head
The head of the femur is considered a problem area where there is an increased risk of arterial blockage and cumulative damage caused by overload and household injuries. The presence of various pathological processes can provoke aseptic necrosis of the thigh.
The main reasons include long-term use of hormonal drugs and antibacterial agents. And also, if a person abuses alcohol, he is often in a stressful state. The provoking factor may be the presence of congenital hip dislocation, osteopenia, osteoporosis, systemic lupus erythematosus, ankylosing spondylitis, rheumatoid arthritis.
The majority of cases have a disappointing orthopedic prognosis and the presence of severe deforming arthrosis. In such a situation, the patient is prescribed endoprosthetics, joint arthrodesis or corrective osteotomy. If magnetic resonance imaging is performed in a timely manner, the disease can be detected at an early stage, which can be treated using conservative methods.
Disability
ANGKB affects all areas of life: health, performance, socialization. With a long duration of the disease at different stages of conservative treatment, patients were forced to change activities with increased physical activity. They choose professions that do not require long periods of being on their feet, moving, or close to their place of residence.
The disability group of such people is determined during a medical and social examination in accordance with the Appendix to the Order of the Ministry of Health of the Russian Federation dated January 27, 1977 No. 33 to the Resolution of the Ministry of Labor and Social Development of the Russian Federation dated January 27, 1977 No. 1: “Classifications and temporary criteria used in the implementation of medical social expertise".
Disability is assigned based on the severity of the disease and decreased quality of life. Changes in the level of disability were carried out only in the case of surgical intervention.
In other words, surgical intervention is most effective in treating aseptic necrosis. Despite the impressiveness of conservative treatment methods, proven effectiveness is questionable.
What is necrosis of the hip and knee joints
The hip joint includes the acetabulum and the head of the femur. The hip joint is the largest ball-and-socket joint in the human body. It is supplied by a single artery passing through the neck of the femur.
If blood circulation is disrupted, the blood supply to the area will be disrupted, and oxygen and nutrients will not be supplied, and bone tissue will lose its properties. The recovery process will become impossible, osteoarthritis will appear, which is accompanied by severe pain.
After some time, necrosis of the hip joint develops. In such a situation, the patient needs to replace the damaged joint. For this, an artificial analogue is used. The procedure is called endoprosthetics, when motor activity is completely restored.
Destructive processes in the knee joint occur as a result of injury and loss of blood supply. The joints lose their functions, and the person may become disabled. With aseptic necrosis of the knee joint, a person experiences severe pain and observes that the motor ability of the knee has decreased. Magnetic resonance imaging and bone scanning can detect early changes, thereby preventing further bone loss.
Using non-steroidal anti-inflammatory drugs can get rid of pain and reduce inflammation. If a person is indicated for surgery, a bone transplant will be performed.
What is necrosis of the talus and humerus?
With this disease, painful sensations appear in the shoulder joint, its movement is limited, as a result of which the risk of atrophy increases. A rare phenomenon includes an altered structure of the humerus. As the disease progresses, the patient is prescribed surgical intervention, which is called endoprosthetics. In this situation, this is the only way to restore lost functions of the upper limbs.
Necrosis of the talus occurs spontaneously and rapidly progresses. With degenerative changes in the ankle joint, deforming arthrosis develops. Thanks to modern diagnostic methods used in the medical center, it is possible to determine the early stage of changes in the ankle joint. In such a situation, mosaic osteochondroplasty is used, as a result of which the anatomy of the joint is restored.
Sources
- Bondarenko O.N., Ayubova N.L., Galstyan G.R., Dedov I.I. Transcutaneous oximetry in dynamic monitoring of patients with diabetes mellitus and critical ischemia of the lower extremities. Diabetes. 2013;16(1):33-42.
- Mitish V.A., Paskhalova Yu.S., Ushakov A.A., Slepnev S.Yu., Mishurinskaya E.A. The role of disarticulation and guillotine amputation of the leg in the strategy of surgical treatment of ischemic gangrene of the lower limb. Wounds and wound infections. Journal named after prof. B.M. Kostyuchenka. 2020;7(1):26-35.
- Barkhatova N.A., Abdulova Yu.B. Some clinical and laboratory risk factors for death in gangrene of the extremities. //Innovative science. - 2021. - No. 4.
Diagnostic measures
If necrosis is suspected, the patient may be sent for an X-ray examination. However, it should be taken into account that this method does not detect pathology at the initial stage of development. An X-ray can reveal pathology if it has progressed to the second or third stage. During the study of this disease, taking a blood test will also not bring an effective result. Thanks to modern devices that are used for magnetic resonance and computed tomography, it is possible to detect changes in tissue structure in a timely manner and with maximum accuracy.
How does necrosis end?
A favorable outcome of the pathology will be with enzymatic melting of tissues, germination of connective tissues into the remaining dead tissue, followed by the formation of a scar. The area of necrosis can become overgrown with connective tissue, resulting in the formation of a capsule. In addition, bone can form in the dead area. This phenomenon is called ossification.
An unfavorable outcome of the pathological condition is characterized by purulent melting, as a result of which the risk of bleeding and spread of the lesion increases. This is how sepsis will develop.
With ischemic stroke, myocardial infarction, necrosis of the kidney or pancreas, that is, when vital organs are affected, there is a high probability of death.