General information
Orchiepididymitis (syn. epididymo-orchitis) is a combined inflammation of the testicle and epididymis of various etiologies. ICD-10 orchiepididymitis code: N45.9. It is one of the most common diseases of the scrotal organs, which can develop as an independent disease or appear against the background of another pathology. Recently, there has been a clear trend toward an increase in the incidence of scrotal organs of infectious and inflammatory origin (acute orchitis , epididymitis , testicular torsion , hydrocele , scrotal trauma). It has been established that nonspecific acute orchiepididymitis occurs in almost 80% of patients with testicular inflammation.
testosterone are produced in the testicles , and their maturation occurs in the epididymis. Triggers of the inflammatory process in the testicles/appendages are predominantly urethritis and prostatitis . According to various authors, the pathology is most common in men aged 20 to 40 years, there is pronounced seasonality, there is no endemicity, and no racial priorities have been identified. The disease develops primarily as a result of infection entering the testicle/epididymis through the hematogenous or lymphogenous route.
The problem is quite relevant since acute epididymitis orchiepididymitis on the right/left, being an urgent disease, requires quick diagnosis and adequate treatment. Delay/inadequate treatment of the acute process contributes to its transition to a chronic course, which can cause sclerotic/dystrophic changes in the testicle and its epididymis, causing obstruction of the vas deferens, which is accompanied by a high risk of impaired male reproductive function.
Treatment: how it goes
Treatment of orchiepididymitis must begin at the first symptoms, so the prognosis for a quick and complete cure is most favorable. Treatment takes place in a hospital setting and the doctor monitors the healing process on a daily basis. The man is prescribed bed rest and wearing special underwear that will pull the affected testicle up.
Conservative method
After testing and identifying the pathogen, the doctor will prescribe an antibiotic that will eliminate the infection. At the same time, cold compresses should be applied to the sore testicle, which will eliminate discomfort and help relieve swelling. When treatment for acute epididymitis orchioepididymitis is completed, the patient will begin to attend physical procedures (magnet, ultrasound, electro and laser therapy) to restore the ability of the testicle to function normally.
Surgical method
Particularly complex conditions require surgical treatment of orchiepididymitis. It is necessary to act radically in cases where complications have developed - blockage of the vas deferens, abscess in the scrotum, fistulas, testicular infarction, infertility, oncological process.
Pathogenesis
In the pathogenesis of the disease, the leading role is given to the introduction of an infectious agent (specific/nonspecific) into the testicle or epididymis by the hematogenous/lymphogenous route. The inflammatory process contributes to compression of the testicular tissues by the accumulation of exudate and disruption of lymph/blood flow. In the pathogenesis of orchiepididymitis, a significant role is also played by transient immunological disorders, namely, the process of suppression of cellular immunity, the appearance of agglutinating sperm antibodies of the IgG/IgM class, a significant increase in the concentration of IgG, as well as immunomobilizing antibodies, etc., which indicates the transformation of serous inflammation into infectious destructive process.
Treatment of inflammation of the testicle and its epididymis (orchitis and epididymitis) in Voronezh
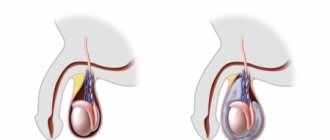
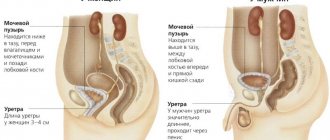
The testicles are a paired organ located in the scrotum. Its main functions: the production of testosterone (through which a man’s sexual and social ambitions are realized) and sperm (through which the transfer of male genetic material is realized). Therefore, often complications or consequences of orchitis (inflammation of the testicle) are impotence and infertility. The appendage is an organ in the form of a dense cord adjacent to the side of the testicle. Sperm maturation occurs in this organ. Therefore, complications or consequences of epididymitis (inflammation of the appendage) are often infertility. As a rule, orchitis and epididymitis occur and develop together (inflammation easily spreads from the testicle to the epididymis and vice versa). Therefore, the diagnosis and treatment of these diseases are no different from each other, and will be discussed further in the article in one block.
Causes of orchitis and epididymitis:
1. Infection . The testicle is an organ isolated from the environment. Therefore, when inflammation appears in it (and the cause of inflammation is usually an infection), the question naturally arises: where did it come from? The prostate is often the source of infection. When there is inflammation in it (prostatitis), the infection travels down the vas deferens into the testicle. However, the immunity in the testicle destroys the normal microflora without problems. There are microorganisms - chlamydia, ureaplasma, trichomonas and gonorrhea, which “break through” the immune system and cause inflammation. Diagnosis of prostatitis and STDs is a key point in identifying the causes of inflammation of the testicle and its epididymis.
2. Hypothermia . With prolonged low temperatures or sudden changes in temperature, immunity in the testicles decreases to a critical level. An infection that gets into the testicle (even a normally non-pathogenic microflora), due to the same prostatitis, receives excellent conditions for reproduction and causes inflammation. Identifying hypothermia in the patient's history is extremely important for correct diagnosis.
3. Trauma . Athletes, participants in road accidents and simply people who have received a domestic injury to the testicles are at risk of developing orchitis and epididymitis. During injury, the so-called blood-testis barrier (the barrier between blood plasma and testicular tissue) is destroyed. As a result, the body begins to produce antibodies (killer cells) to the testicular tissue - a severe, autoimmune form of orchitis develops, often leading to infertility.
There are acute (disease duration no more than 2 months) and chronic (disease duration more than 2 months) orchitis and epididymitis.
Symptoms (signs) of acute orchitis and epididymitis
1. Severe pain in the testicle or scrotum, preventing even walking 2. Increased (over 37°) temperature 3. General intoxication: weakness, malaise, loss of appetite, sweating, chills 4. On examination - the testicle is sharply enlarged in size, purple-cyanotic colors, painful to the touch
Symptoms (signs) of chronic orchitis and epididymitis
1. Periodic, dull aching pain in the testicle or scrotum, intensifying after sex or physical activity. 2. Upon examination, the testicle and epididymis are compacted, lumpy, the epididymis is fused to the testicle
Possible complications (consequences) of orchitis and epididymitis
1. Transition of inflammation to the purulent stage with the development of a testicular abscess . The time factor plays a key role here. If acute orchitis lasts more than 3 days, the likelihood of developing purulent melting of the testicle increases sharply. There is only one treatment at this stage - surgery (decompression of the testicle or its resection, up to complete amputation in severe cases).
2. Chronic inflammation . As a rule, this is facilitated by patient self-medication. Taking the wrong antibiotics, in the wrong doses and for the wrong duration, leads to the elimination of the symptoms of the disease and creates a false sense of complete recovery in the patient. However, orchitis remains and turns into a chronic, relapsing form, in which periods of exacerbation (obvious symptoms) are followed by periods of remission (calm).
3. Impotence . Often a consequence of chronic orchitis. Decreased testosterone production caused by chronic inflammation of the testicle underlies severe, endocrine, form of impotence. This form of erectile dysfunction is quite difficult to treat.
4. Infertility . Occurs in 30-40% of patients who have suffered acute orchitis and epididymitis and in 50-70% of those with chronic epididymitis. The reason is both a decrease in the production of sperm that is normal in quantity and quality, and a disruption in the transportation of sperm along the vas deferens to the urethra, due to the formation of adhesions. Treatment is lengthy and extremely costly, both in time and finances.
Treatment of orchitis and epididymitis with folk remedies and at home
It is absolutely ineffective and extremely dangerous due to the high probability of developing a purulent stage of orchitis or its chronicity (loss of time and development of resistance to antibiotics in microorganisms). The testicles are a vital organ for a man, and experiments with self-medication can have very detrimental consequences, both for potency and his reproductive function.
How do I treat orchitis and epididymitis?
1. Treatment of acute orchitis and epididymitis.
If the first symptoms are detected, an urgent consultation with a urologist is necessary!
A big role here is played by the timeliness of the diagnosis and differentiation of the situation when the process has already entered the purulent stage and surgery is required. Narrow-spectrum antibiotics with tropism (directionality) to testicular tissue are prescribed. This gives a quick and pronounced effect. As a rule, a clinical response (a sharp improvement in the patient’s well-being) occurs on the 3rd day. Subsequently, medications are prescribed to help completely relieve inflammation and restore testicular function.
2. Treatment of chronic orchitis and epididymitis
After establishing a diagnosis and identifying the causes supporting the chronic inflammatory process (STDs, adhesions, etc.), a course of treatment is prescribed. Several courses lasting 2-3 weeks are conducted at intervals of 3 months. This scheme allows the testicular tissue to regenerate as much as possible and restore lost function. The course includes drugs that improve microcirculation, testoprotectors (drugs that improve testicular regeneration) and absorbable medications. In addition, to enhance the effect, physiotherapy is prescribed: laser, magnet, ultrasound. In most cases, depending on the stage of the disease, within 6-12 months. there is a pronounced clinical improvement.
Cost of treatment
Examination and treatment are carried out according to medical standards
1. Acute orchiepididymitis
• Initial appointment (gathering complaints, medical history, clinical examination, making a preliminary diagnosis, prescribing an examination program) - 1000 rubles. • Basic examination (UAC, OAM, ultrasound of the scrotum, examination for STDs) - 3,500 rubles. • Repeated appointment (analysis of examination results, making a final diagnosis, prescribing a treatment regimen) – 600 rubles. • Treatment: Medicines - antibiotics (injectable forms) and anti-inflammatory drugs - on average 3,000 rubles per course. After eliminating the main inflammation for 3 months. restorative therapy - 1500-2000 rubles/month. (drugs that stimulate regeneration). If necessary, a course of physiotherapy is carried out. • Cont. tests (OAC, OAM, ultrasound of the scrotum) after 3 months. – 1000 rub.
2. Chronic orchiepididymitis
• Initial appointment (gathering complaints, medical history, clinical examination, making a preliminary diagnosis, prescribing an examination program) - 1000 rubles. • Basic examination (CBC, OAM, ultrasound of the scrotum, TRUS, total testosterone, spermogram, PCR for STDs) - 5,000 rubles. • Repeated appointment (analysis of examination results, making a final diagnosis, prescribing a treatment regimen) – 600 rubles. • Treatment: For 1 course (2-3 weeks) - medications (very average) - 2000 rubles. + physiotherapy – 1000 rub.\ session 10 sessions. From 1 to 3 courses are carried out depending on the speed of regeneration and the degree of functional restoration in a particular patient. • Cont. tests (OAC, OAM, ultrasound of the scrotum) at the end of each course - 1000 rubles.
When to see a doctor
A 19-year-old man complained of acute severe pain in the right testicle, weakness, malaise and fever up to 38°. Sick for 7 days after swimming in the ice hole for baptism. On examination, the right testicle is sharply painful to the touch, the skin of the scrotum is bluish-purple in color. Ultrasound of the scrotum shows diffuse inflammation of the right testicle with transition to the right appendage and the formation of a focus of purulent melting (abscess). Due to the fact that time was lost, the patient was urgently hospitalized in the on-duty urology department, where he underwent surgery (testicular decompression). Thanks to the professionalism of my colleagues, the testicle was saved. After discharge from the hospital, the condition lasted for 6 months. course of rehabilitation treatment with a diagnosis of chronic orchiepididymitis. After 6 months The examination results were for the most part normal. PS after recovery, the patient promised not to swim in bodies of water for baptism anymore
Classification
Based on the nature of the inflammatory process, they are divided into:
- a specific form of the disease (the etiological factor is specific pathogens of tuberculosis , gonorrhea , syphilis , brucellosis );
- a nonspecific form of the disease (caused by protozoa ( Trichomonas ), bacteria ( Escherichia coli , cocci , mycoplasmas , Proteus , chlamydia , Klebsiella rubella and mumps viruses , influenza , enteroviruses .
According to the form of the inflammatory process: acute (serous/purulent) and chronic.
By localization, one-sided (right/left) and two-sided.
By severity:
- Mild - duration does not exceed three days.
- Medium - duration up to six days, accompanied by severe symptoms (pain, increased body temperature up to 39°C).
- Severe - with a duration of more than seven days, accompanied by severe symptoms.
Treatment of acute and chronic orchitis and orchiepididymitis
The treatment regimen is drawn up taking into account the patient’s complaints, symptoms, laboratory and instrumental research data. Depending on the course and root cause of the disease, treatment can be conservative or surgical.
Conservative therapy
- Antibiotics
- Anti-inflammatory
- Anesthetics
- Physiotherapy
- Operative therapy
Since diseases in most cases develop against the background of an infectious lesion, treatment is carried out with antibiotics, which are chosen based on the results of microflora culture.
In addition to antibiotics, the urologist prescribes non-steroidal anti-inflammatory drugs: Indomethacin, Diclofenac, Celebrex. These medications quickly reduce swelling, pain and relieve inflammation.
If the patient complains of severe pain, the doctor performs a blockade of the spermatic cord.
After the severity of the process has been relieved, various types of physiotherapy can be used to speed up the healing process and have an anti-edematous effect.
IMPORTANT: during therapy it is recommended to wear supportive swimming trunks.
When diagnosing recurrent orchiepididymitis or abscesses on the testicle or its epididymis, an operation is performed to open the abscess, or completely remove the testicle or epididymis in difficult cases.
Make an appointment
Causes
Orchiepididymitis is a polyetiological disease. The main reasons include:
- Infectious and inflammatory diseases (acute/chronic) of the genitourinary tract - prostatitis , urethritis , STDs ( chlamydia , syphilis , gonorrhea ).
- Complications after common infectious diseases ( influenza , tuberculosis , tonsillitis , mumps , brucellosis , etc.).
- Injuries to the scrotum, instrumental intervention ( cystoscopy , bougienage , catheterization ), complications after surgical interventions on the prostate.
- Inflammatory diseases in the pelvis ( paraproctitis , varicose veins , hemorrhoids ).
- Congestion that develops as a result of testicular torsion, wearing tight underwear, prolonged erection without ejaculation, compression of the scrotal organs when working in a sitting position, masturbation, sexual excesses.
Predisposing factors are alternative types of sex, weakened immunity, frequent hypothermia, prolonged stress, increased sexual activity or its long-term absence.
Causes of development of orchiepididymitis
The cause of orchiepididymitis, like any other inflammatory process, is infection by microbes. Usually these are Trichomonas, causative agents of chlamydia and other STIs. They enter the testicle from the urethra or prostate through the bloodstream or through the vas deferens.
In other cases, the source of microbes is inflammation of the urethra, injury to the testicles.
The development of this pathology is promoted by blood stagnation in the pelvis, hypovitaminosis, perineal trauma, and prostate surgery (occasionally).
Symptoms
Acute orchiepididymitis on the right and acute orchiepididymitis on the left manifests itself with a high temperature (39-40°), a sharp pain syndrome radiating to the lower abdomen/lower back, aggravated by walking. Associated symptoms include weakness, general weakness, myalgia . On examination, there are signs of local inflammation - the scrotum on the side of the disease increases significantly in size, the folds are smoothed out, the skin of the scrotum becomes tense/shiny, and erythema is often present. When touched there is a sharp pain. Dysuria is typical ; patients complain of pain when urinating. In most cases, there is discharge from the urethra, often purulent and with an unpleasant odor.
In the absence of adequate and timely treatment, especially against the backdrop of weakened immunity, acute serous inflammation may transform into purulent epididymo-orchitis , which manifests itself as severe general intoxication with damage to the genitourinary system, and is also accompanied by the risk of developing a bilateral process.
With the transition to a chronic process, the severity of symptoms of orchiepididymitis decreases: a prodrome is characteristic, moderate pain in the scrotum, which intensifies with movement or palpation. The scrotum is compacted, and there is a discharge of impurities/red blood cells with an unpleasant odor in the semen. Patients complain of decreased libido .
Recommendations of urologists and prevention
Experts urge men not to ignore the symptoms of acute orchiepididymitis, not to treat themselves, and not to endure pain and discharge from the genitourinary canal. You should immediately consult a doctor for medical help, because the sooner treatment for epididymitis orchioepididymitis is started, the greater the chances of a successful recovery. If treatment is started on time, the recovery period will take several days.
Prevention measures
You can prevent the development of the disease by following your doctor's recommendations. Sexually transmitted infections are the cause of the development of epididymitis orchioepididymitis in men. Using a condom during sexual intercourse will reduce the risk of infection. And injuries to the external genitalia can provoke the development of infection, in which case you should definitely visit a doctor for diagnostics. Also, the testicles need to avoid hypothermia, wear underwear made of natural fabrics, and treat genitourinary diseases in a timely manner so that there are no complications in the future.
Tests and diagnostics
The clinical diagnosis is made on the basis of anamnesis, the results of an objective examination of the scrotal organs and data from laboratory and instrumental examinations. Examination for orchiepididymitis includes:
- Laboratory research methods: bacteriological examination of urine, biochemical blood test, CBC, OAM, urethral smear, bacteriological examination of sperm/prostate juice (with determination of sensitivity to antibiotics).
- PSA blood test.
- PCR (if necessary).
- Instrumental research methods: ultrasound of the scrotum, urethroscopy.
It is mandatory to examine not only the patient, but also his sexual partner.
Prices for services
Initial appointment with a urologist FOR MEN + ultrasound of the prostate gland (assessment of complaints, medical history, if necessary, rectal digital examination, ultrasound of the prostate gland in men)
Primary appointment – visiting a doctor of a specific specialty for the first time. Includes a conversation with the patient, an initial examination, anamnesis, if necessary, a digital rectal examination, and an ultrasound of the prostate gland. The price is valid from 02/01/2021 The price is not valid for appointments at the branches of Bolshevikov Ave. and Prosveshcheniya Ave. Make an appointment
550 ₽
Initial appointment with manager Department of Urology Rylchikov I.V. + Ultrasound (includes a conversation with the patient, initial examination, medical history, if necessary, rectal digital examination, ultrasound of the prostate gland)
Primary appointment – visiting a doctor of a specific specialty for the first time. Make an appointment
1200 ₽
Repeated appointment with the urologist
Make an appointment
700 ₽
Prevention
There is no specific prevention of orchiepididymitis. As general preventive measures, we can recommend:
- Use barrier contraception during casual sexual intercourse.
- Practice a healthy lifestyle (rational nutrition, quitting smoking, abusing alcoholic beverages, playing sports, conditioning the body).
- Have a regular sex life.
- Avoiding sitting for long periods of time.
- Boosting immunity.
- Timely treatment of STIs ( prostatitis , urethritis ), infectious diseases.
- Avoid hypothermia.
- Avoid injury to the scrotal organs.
Contraindications
You cannot have sex during the course of the disease, as well as during its treatment. This can cause infection of the partner and also lead to complications.
Also, you should not visit the sauna, go to the pool, avoid physical activity and swim in a pond in order to prevent the disease from getting worse and to prevent excessive infection activity.
Only after comprehensive and complete treatment of orchiepididymitis can you return to your normal lifestyle.
Consequences and complications
In the absence of adequate/timely therapy, the risk of impaired spermatogenesis and the development of difficulties in sperm transport increases. The risk of infertility increases significantly with bilateral orchiepididymitis, which is manifested by insufficient production of the male sex hormone ( testosterone ) and, as a consequence, androgenic insufficiency, manifested by decreased libido (sexual desire), insufficient erection, decreased performance, and decreased muscle mass.
Possible complications
Possible complications include:
- transition to a chronic form with improper or absent treatment;
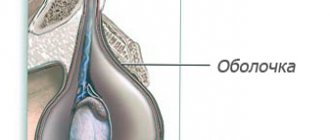
- development of reactive hydrocele (often occurs during the course of the disease and disappears after treatment);
- suppuration of the tissue structures of the testicle;
- testicular tissue atrophy;
- development of infertility;
- erection problems;
- decreased libido due to decreased testosterone production.
To avoid the development of the above complications, you should immediately contact a urologist at the first symptoms, diagnose the disease and begin its treatment.
List of sources
- Akkaliev M.N. Acute orchiepididymitis: modern aspects of etiology, diagnosis and treatment. Literature review // Science and Healthcare. 2021. No. 2. P. 159-175.
- Inflammatory diseases of the genital organs in men. Guidelines. Ed. M.P. Kogan and G.G. Selezneva. Rostov-on-Don; 2011.
- Bashembaev Kh.M., Nazarkulov E.N. Choice of treatment method for patients with acute inflammatory diseases of the epididymis and testicle // Bulletin of the Almaty State Institute for Advanced Medical Studies. 2010. No. 2 (10). pp. 35-37.
- Naber K.G., B. Bergman B., Bishop M.K. Recommendations of the European Association of Urology for the treatment of urinary tract infections and infections of the reproductive system in men // Clinical microbiology and antimicrobial therapy. 2002. No. 4, Volume 4. P. 347-363.
- Vorchalov M.M. An integrated approach to the treatment of acute epididymo-orchitis: dissertation. ...cand. honey. Sci. Saint Petersburg. 2013. P. 140.
Treatment of epididymitis orchioepididymitis at GUTA CLINIC
Treatment of epididymitis orchioepididymitis at GUTA CLINIC
carried out in accordance with international standards for the treatment of urological diseases. When prescribing a treatment regimen for orchiepididymitis, the urologist takes into account many factors - the form and degree of the disease, the general health of the patient, tolerability of certain medications, the presence of concomitant diseases, etc.
Treatment of acute form of orchiepididymitis
involves the use of complex antibacterial therapy aimed at eliminating the causative agent of the disease, as well as conservative treatment methods - bed rest, drinking plenty of fluids and other measures.
Treatment of chronic orchiepididymitis
depending on the degree of advancedness of the disease, it may include pharmaceuticals, physiotherapeutic procedures, antibiotic therapy, etc.
Prevention of the development of orchiepididymitis includes recommendations for strengthening the immune system, treating existing concomitant diseases (especially for STDs and general diseases), playing sports, vitamin therapy and other measures.
It is very important to properly treat epididymitis orchioepididymitis
. You should not trust the recommendations of a pharmacy specialist or the advice of a close friend - antibacterial drugs are always prescribed individually, strictly according to indications. Trying to get rid of the disease, you can seriously harm your body.
That is why it is best to entrust the treatment of orchiepididymitis
professionals - certified urologists from GUTA CLINICS will help you maintain men's health and well-being for many years!