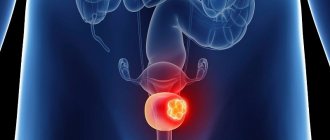
What is commonly called "testicular cancer" is not actually cancer, but another malignant tumor of the testicle. Cancer develops exclusively in the epithelial tissue that forms the mucous membranes; no mucous membrane means no cancer, but there is a malignant tumor.
Cancer in the testicle also happens, but this is a special embryonic cancer that develops in an adult man from the gonadal epithelium; it is classified as germ cell malignant testicular tumors. It is assumed that germ cell tumors are formed during the period of embryonic development in the womb, when in the first half of pregnancy the fetal germ cell acquires malignant potential.
- Causes of development and risk factors for testicular tumors
- Classification. Types of testicular tumors
- Symptoms of testicular tumors
- Diagnosis of testicular cancer
- Testicular cancer treatment
- Prognosis for testicular cancer
- Prevention of testicular cancer
- Prices for treatment at Euroonco
Malignant testicular tumors are not very common, accounting for no more than 2% of all malignant neoplasms, but over the past 2–3 decades they have shown a doubling of incidence. Russians suffer from malignant testicular tumors 4 times less often than Europeans, however, in terms of the rate of annual increase in incidence, tumors are firmly in the top, occupying second place. Fortunately, today up to 90% of patients are cured from testicular cancer, which is not cancer at all, but another malignant tumor.
Their distribution is inexplicable. No one will say why the Spaniards and Portuguese get sick 5 times less often than the Danes, and even the Finns closest to Denmark suffer from testicular cancer 4 times less often. White-skinned men are more prone to malignant testicular tumors; they are not at all typical for black men. The main concern is that young men aged 15 to 44 years suffer from malignant testicular tumors.
With a steady increase in incidence, since the 1970s, mortality from malignant testicular tumors has decreased almost fourfold. In the twentieth century, mortality from testicular tumors increased exactly until the entry of platinum drugs into the pharmaceutical market, which brought about a chemotherapeutic revolution. Platinum drugs have been greatly helped by new diagnostic techniques, and especially by the determination of tumor markers. All this together ensures an extremely low mortality rate: one per 300 thousand male population.
Symptoms
The first signs of testicular cancer do not appear immediately. In the early stages, the course of the disease is usually asymptomatic, only sometimes a feeling of heaviness appears, and changes in the size of the testicle or scrotum are observed. This is already a reason to immediately contact a urologist and undergo an examination.
As the disease progresses, the following symptoms and signs of testicular cancer may appear (in increasing order):
- pain in the scrotum;
- the appearance of a compaction that can be felt independently;
- change in the consistency of the testicle (when compared with another) - the patient can also feel this himself;
- pain in the back - from this sign onwards we talk about symptoms characteristic of the course of the disease during metastasis;
- swelling of the lower extremities;
- problems with urination, kidney function;
- shortness of breath and cough with lung damage;
- enlarged supraclavicular lymph nodes.
If treatment for testicular cancer is not started in time, metastases will spread very quickly, undermining a man’s health.
Sometimes it happens that the symptoms of testicular cancer are accompanied by additional changes due to severe hormonal imbalances. In this case, there are a number of other signs:
- gynecomastia - that is, enlargement of the mammary glands in a man;
- erectile dysfunction and decreased libido in adults;
- frequent and long erections in boys - the symptom is precisely the duration and frequency, and not the fact of erection itself, which is normal for boys;
- premature enlargement of the penis, as well as early appearance of pubic hair;
- development of bones and muscles that advances with age.
Even taking into account the fact that there are many symptoms, you should not wait until the body reports serious problems. The first signs of testicular cancer in the form of a feeling of heaviness and changes in size already indicate that urgent qualified help is needed.
Prevalence of the disease
Among young men (aged 20-40 years), testicular cancer is the most common malignancy. The incidence has increased over the past few decades in industrialized countries. Testicular cancer affects 1 in 300 men during their lifetime, but 1 in 5,000 die from it. The low mortality rate compared with the incidence is due to the fact that, unlike most other forms of cancer, testicular cancer responds well to treatment and has a favorable prognosis. Most men with this diagnosis are successfully cured
and forget about the disease forever.
Causes and risk factors
Risk factors potentially affecting testicular cancer in men include:
- heredity;
- scrotal injuries;
- undescended testicle or congenital underdevelopment of the testicles;
- nevi and moles that can develop into malignant formations;
- diseases of endocrine pathology;
- radiation, radiation, chemical exposure;
- constant overheating of the scrotum;
- early puberty in a boy;
- unhealthy lifestyle: abuse of nicotine, alcohol, lack of activity.
Most often, tall men with a thin build, as well as representatives of the white race, are susceptible to cancer of the epididymis and the testicle itself.
Classification. Types of testicular tumors
Testicular tumors are very diverse in their cellular structure, but 90–95% of them belong to the group of germ cell tumors:
- intratubular neoplasia;
- yolk sac tumor;
- seminoma;
- teratoma;
- trophoblastic tumor (choriocarcinoma);
- embryonal cancer;
- mixed tumors
The remaining 5–10% are benign and malignant Leydig or Sertoli cell tumors, adult and juvenile granulosa cell tumors, theca fibromas and mixed ones.
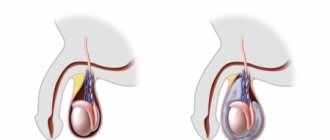
Giving rise to cancerous invasion - the penetration of cells through the restrictive basement membrane - intratubular neoplasia (TIN) or carcinoma in situ is often found in the surroundings of a testicular tumor, and in 2-5% of patients it is found even in a healthy testicle, so its treatment is very serious. Since four out of 10 germ cell tumors are seminomas, and the rest are all other histological types with the same response to treatment, all testicular germ cell tumors (GCTs) are clinically divided into two groups: seminomas and non-seminomas, which are treated differently.
Stages
One of the classifications used by oncologists distinguishes four stages of testicular cancer:
- 1st. Swelling and pathological nodules are observed only in one part of the scrotum.
- 2nd. The neoplasms grow (from 2 to 5 cm), and nearby lymph nodes are involved in the process.
- 3rd. The tumor is clearly visible even without special devices. Lymph nodes on the chest and neck are enlarged.
- 4th. Metastases are observed in various organs and tissues, including the brain. Treatment consists of palliative support.
The first and second stages of the disease are most favorable for treatment.
Materials of congresses and conferences
Testicular cancer: clinical picture and stages of the disease.
William G. Jones Leeds Teaching Hospital NHS Trust, Cookridge Hospital, Leeds, UK
Clinical picture.
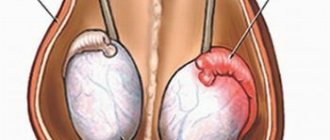
Testicular cancer is a relatively rare tumor, and usually practicing doctors rarely encounter this pathology. As a rule, testicular cancer affects men of working age from 15 to 50 years [1]. The clinical picture of the disease consists of symptoms caused by the presence of a primary testicular tumor and metastases, or a combination of them. The most common signs of a primary testicular tumor are pain, enlargement or swelling of the organ with the appearance of a palpable tumor formation in it. These symptoms occur in 80-90% of patients [2]. Only 10% of patients complain of pain, often severe, indicating infringement of tumor masses, bleeding or infarction in the tumor tissue, or concomitant acute epididymitis. Patients often have a history of recent trauma to the scrotal area. Patients may also report that the affected testicle has recently changed in consistency and size, becoming denser, or, less commonly, becoming softer and smaller (due to atrophy). Often patients note a feeling of heaviness in the scrotum or dull pain in the lower abdomen or scrotum area. Often the patient’s sexual partner is the first to discover a mass in the testicle and insist on consulting a doctor. In 5% of cases, the only symptom of the disease may be back pain. This is a very common and nonspecific symptom in this age group, but it may be a manifestation of metastatic testicular cancer [3]. About 3% of patients have signs of gynecomastia, which occurs as a result of the secretion of significant amounts of human chorionic gonadotropin by tumor tissue [4].
Often the symptoms associated with the presence of metastases prevail over the symptoms of testicular damage. Severe back pain may indicate enlargement of the retroperitoneal lymph nodes, which compress the nerve roots, or involvement of the lumbar muscle in the process. Gastrointestinal symptoms and weight loss are common, and sometimes a tumor mass is detected by palpation in the abdominal cavity. The spread of the tumor above the diaphragm can lead to the detection of visible tumor masses in the left supraclavicular region and complaints of shortness of breath and chest pain [5]. Very rarely, patients complain of bone pain resulting from metastatic skeletal lesions. When the central nervous system is involved, symptoms of increased intracranial pressure, epileptiform seizures, or other neurological symptoms appear. More than 50% of patients with nonseminoma and 25% with seminoma have metastases when visiting a doctor, which are clinically manifested in only 10% of cases.
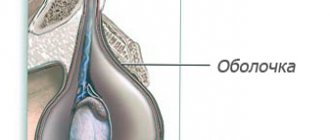
Ultrasound diagnostics can be used for the differential diagnosis of various pathological formations in the scrotum [1,6]. Because testicular cancer has a short cell doubling period (an average of 3 weeks for non-seminoma), the tumor can grow in size very quickly. Therefore, it is especially important to promptly refer such a patient to a specialist. This is especially true for patients with prolonged hydrocele failure to resolve or patients with epididymo-orchitis who have not responded to antibiotic therapy for more than 2 weeks. Differential diagnosis of testicular cancer includes epididymo-orchitis, testicular tuberculosis, granulomatous orchitis, hydrocele, hematocele, hematoma or hernia, as well as gumma and testicular torsion. However, any testicular mass should be considered as a possible testicular cancer, and any patient with suspected testicular malignancy should be immediately evaluated by a urological surgeon or oncologist [1].
Untimely (late) diagnosis.
Delay in diagnosis is rare and usually occurs due to the patient’s delay in visiting a doctor [7-10]. It is clear that late diagnosis leads to the need to treat a more widespread disease and, accordingly, to a worse prognosis. Patients put off visiting a doctor for various reasons: firstly, it is the fear of a sexually transmitted disease (especially in the case of adultery), and secondly, the fear that treatment may disrupt their sexual function. A small proportion of patients are embarrassed to discuss this issue or even allow a doctor to examine them, especially if the doctor is a woman.
Popular educational programs are needed to reduce public ignorance on this issue and reduce the incidence of late diagnosis [11]. They should explain the seriousness and potential risk of this disease in men aged 15 to 50 years, teach self-examination techniques and show the real possibility of cure if they consult a doctor in a timely manner. On the other hand, doctors should always remember that any tumor formation in the testicle should be regarded as malignant until proven otherwise. An example is the reporting of a cyclist who achieved victory in last year's Tour de France after being cured of testicular cancer. Information about this case helped reduce public ignorance and social taboos against discussing the issue in the press.
Examination of the patient.
The patient's examination begins with careful palpation of the testicle. Normally, the testicles have a dense but homogeneous consistency and are quite mobile. The epididymis is usually palpated as a separate formation. A testicular tumor is usually suspected when the testicle becomes denser and increases in size. Less commonly, the testicle becomes atrophic and decreases in size. As the examination continues, palpation of the groin, abdomen and supraclavicular areas is performed in order to exclude metastatic lesions of the lymph nodes in these areas. The examination would not be complete without a clinical examination of the chest organs and examination of the mammary glands.
Ultrasound examination (ultrasound) of the scrotum area should be included in the examination of a patient with suspected testicular malignancy and can be easily performed in any hospital. Ultrasound is a non-invasive, relatively inexpensive method that can distinguish normal testicular tissue from tumor formation in almost 100% of cases. Magnetic resonance imaging (MRI) is a more accurate method, but cannot be used in routine practice due to the high cost of the method. However, in some cases, MRI can be used to resolve discrepancies between ultrasound and physical examination findings. Orchofuniculectomy and histological examination of the obtained material clarify the diagnosis of testicular tumor. This procedure allows you to remove the testicle without damaging the tunica albuginea, which avoids local metastasis or local recurrence.
Testicular cancer staging.
The stage of testicular cancer is determined according to the degree of spread of the process before removal of the primary tumor. As is known, the staging of various malignant tumors differs in different anatomical regions. Testicular cancer metastasizes by hematogenous and/or lymphogenous route. Metastasis occurs through the lymphatic vessels into the retroperitoneal space, mainly in the kidney area. Right-sided tumors preferentially metastasize to the aortocaval, precaval, and right para-aortic lymph nodes, whereas left-sided testicular tumors tend to spread to the left para-aortic and preaortic lymph nodes. About 1/5 of tumors of the right testicle can also metastasize contralaterally to the retroperitoneal lymph nodes on the left, which is not typical for tumors of the left testicle. Subsequently, metastases spread to the lymph nodes of the renal hilum and legs of the diaphragm. Supradiaphragmatic metastasis occurs through the thoracic duct, reaching the upper mediastinal and supraclavicular lymph nodes. Penetration of cancer cells (emboli) through the supraclavicular vein into the pulmonary bloodstream leads to the appearance of pulmonary metastases. Direct lymphatic spread through the diaphragm may lead to metastases in the posterior and inferior mediastinum. Hematogenously, testicular cancer metastasizes to the lungs, liver, bones, bone marrow, and skin. This is more common in nonseminomas than in seminomas.
The task of staging the process is to determine the extent and nature of metastases, which further determines the patient’s treatment tactics. The level of serum markers hCG (human chorionic gonadotropin), AFP (alpha fetoprotein) and LDH (lactate dehydrogenase) should be determined in the pre- and postoperative period, and subsequently at weekly intervals. The situation when, after surgery, the level of AFP and hCG does not normalize, indicates the prevalence of the disease, which makes these serological tests justified. In such a clinical situation, a CT scan (the advantages of MRI have not yet been proven) of the chest, abdominal cavity and pelvis should be performed in the near future after orchofuniculectomy. CT or MRI of the brain is indicated for patients with multiple metastatic foci in the lungs or with a postoperative hCG level of more than 10,000 IU/ml, because they have a high risk of cerebral metastases.
Stages of testicular cancer before 1997
Bypassing the general agreement that stage I disease is the stage when only the testis is affected, different classifications were used in the world before 1997. This inconsistency between individual centers did not allow analysis of the results of various non-randomized studies. With the advent of effective chemotherapy regimens, it became clear that the success of treatment and, accordingly, the prognosis of the disease depend on the extent of the disease. The weight of the metastatic tumor, the number of groups of lymph nodes involved, and the location of metastases are important for prognosis. An increased level of expression of serum tumor markers AFP and hCG also began to be considered as an indicator of the biological aggressiveness of the tumor. There have been many attempts, notably by the EORTC and MRC [13,14], to define prognostic groups of patients. The main task was to develop a classification that would determine the patient's prognosis and the appropriate therapeutic tactics.
Classification.
The anatomical classification proposed by the Royal Marsden Hospital (UK) has been used in the United Kingdom and Europe for more than 20 years (Table 1) [15]. This system reflected the involvement of lymph nodes of various locations in the pathological process, the size and number of pulmonary metastases. Extrapulmonary visceral metastases were classified as stage IV of the disease. This classification continues to be used, although it has recently been modified somewhat. It remains relevant for the management of seminomas and other, rarer types of tumors, such as Leydig cell tumor. Attempts to create a classification with prognostic value led to the creation of a new classification, IGCCCG, in 1997 [16]. This classification was created through the collaboration of clinicians from 10 countries who summarized the experience of treating a large group of patients (5202 patients with non-seminoma testicular tumor and 660 patients with seminoma germ cell tumor) using combinations based on platinum derivatives. A multivariate analysis of the prognostic factors of these patients for survival and progression was performed. As can be seen from Table 2, 3 prognostic groups of patients were identified (good, intermediate and poor prognosis). The three most important prognostic factors were: serum marker levels (including LDH as a prognostic indicator but not a specific marker), the presence or absence of pulmonary metastases, the presence or absence of extrapulmonary visceral metastases, and the presence of extragonadal mediastinal tumor. It is important to emphasize that the group of patients with testicular seminoma included patients for the most part (about 80%) who had stage I or II of the disease and who received radiation therapy more often than chemotherapy. The International Union Against Cancer (UICC) recognized the importance of this work and included this classification in the 5th edition of the international TNM classification in 1997 [17]. The classification summary is presented in Table 3. The stages of the disease are presented in Table 4. This new classification has proven to be a significant aid to clinicians when planning therapy for patients with germ cell tumors.
Symptoms of the disease that are not associated with the main tumor in the testicle.
Backache. Tumor formation in the abdomen.
Patients with testicular cancer metastases to the retroperitoneum suffer from back pain, gastrointestinal disorders (constipation or other symptoms). The patient may not notice a tumor formation in one of the testicles, and if he does notice, then, as a rule, he does not attach much importance to it. Such patients, as a rule, complain of weakness, rapid mental and physical fatigue. Upon further examination, it may turn out that there are tumor metastases in other organs. If the patient is in serious condition, the question of starting chemotherapy before removal of the primary tumor becomes relevant. In such cases, the diagnosis of testicular germ cell tumor is made based on elevated tumor markers.
Extragonadal retroperitoneal germ cell tumors.
A primary extragonadal tumor with an undetectable tumor in the testicle in most cases still turns out to be secondary. Upon careful questioning of the patient's history, there is evidence of mild testicular enlargement over a period of several days or weeks in the past, often occurring many months or even years ago. The mechanism of development of extragonadal tumors in this situation is as follows: the growth of the testicular tumor was so rapid that it outpaced its own angiogenesis, and the tissue of the testicular tumor underwent necrosis, having, however, managed to give metastatic screenings to the retroperitoneal space or mediastinum. Often in such cases, a histological examination after orchofuniculectomy may reveal a scar in the testicle. Upon examination, such a testicle is atrophic, and ultrasound may detect pathology in the testicle [18].
Germ cell tumors of the mediastinum.
About 5-7% of all germ cell tumors develop outside the gonads - in the mediastinum or retroperitoneum. While most retroperitoneal extragonadal tumors are in fact gonadal in origin, mediastinal extragonadal tumors are more often truly extragonadal and have a different nature and biological characteristics from true testicular tumors [19]. For extragonadal nonseminoma germ cell tumors of the mediastinum, the prognosis is completely different, and according to the latest IGCCCG classification, this group of tumors is classified as poor prognosis. Primary seminomas, which account for approximately 30-40% of mediastinal malignancies, have a good prognosis and respond well to standard chemotherapy. A large tumor volume in the mediastinum in such patients is usually discovered incidentally during examination for complaints of shortness of breath or discomfort (pain) in the heart area. Young patients with signs of gynecomastia should undergo chest radiography to exclude a tumor producing hCG.
Other metastatic manifestations.
Patients with aggressive disseminated testicular cancer (usually nonseminoma with trophoblastic elements) may have metastases to any location: brain, liver, bones, bone marrow, skin, lymph nodes of the chest and abdomen, head and neck. Sometimes the diagnosis is made based on a biopsy of material from these lesions. Very often, morphological interpretation is difficult, especially in the case of a tumor with a low degree of differentiation. Morphologists often give the answer “metastases of adenocarcinoma from an undetected primary site.” Therefore, in any young patient with metastatic manifestations of the above localizations, a differential diagnosis with a testicular germ cell tumor should be made. AFP and hCG levels can provide useful information in this situation. When treating such a patient, even in the absence of clear data in favor of this diagnosis, it is necessary to consider the prospect of chemotherapy with the inclusion of platinum drugs.
Table 1.
Royal Marsden Hospital classification [15]
| Stages | |
| I IM | No evidence of disease outside the testicle Increased markers only |
| II IIA IIB IIC IID* | Involvement of lymph nodes below the diaphragm Maximum size Maximum size 2-5 cm Maximum size >5 Maximum size >10 cm |
| III | Involvement of lymph nodes above and below the diaphragm Retroperitoneal lymph nodes A, B, C, as above Medistinal lymph nodes M+ Cervical lymph nodes N+ |
| IV | Visceral metastases Retroperitoneal lymph nodes as in stage II Medistinal or cervical lymph nodes as in stage III Metastases to the lungs: - L1 - L2 multiple metastases with a maximum size - L3 multiple metastases with a maximum size >2 cm Metastases in the liver H+ Metastases to other organs and tissues, please specify additionally |
Table 2.
IGCCC classification. [16]
| Nonseminoma tumors | Seminoma |
| Good prognosis if all signs are present: | |
| Testicular tumor/extragonadal retroperitoneal Metastases to lymph nodes and/or lungs AFP hCG LDH 56% of all patients with nonseminomas 5-year survival rate 92% | Any location of the primary tumor Metastases to the lymph nodes and/or lungs Normal AFP Any hCG Any LDH 90% with metastatic seminoma 5-year survival 86% |
| Moderate prognosis if all signs are present: | |
| Testicular tumor/extragonadal retroperitoneal Metastases to lymph nodes and/or lungs AFP * 1000 and * 10000 ng/ml or CG * 5000 U/L or * 50000 U/L or LDH* 1.5 norms * 10 norms 28% of all patients with non-seminomas 5- summer survival rate 80% | Any location of the primary tumor Metastases to the liver, bones, brain Normal AFP Any hCG Any LDH LDH 10% seminomas 5-year survival rate 73% |
| Poor prognosis if at least one sign is present: | |
| Extragonadal tumor of the mediastinum Metastases to the liver, bones, brain AFP>10,000 ng/ml or hCG>50,000 U/l or LDH>10 normal 16% of all patients with nonseminomas 5-year survival rate 48% | Patients with seminomas do not qualify for a poor prognosis |
Table 3.
1997 TNM classification [17]
| Testicle | |
| PTis pT1 pT2 pT3 pT4 | Intratubular tumor Testis and epididymis, no invasion of venous and lymphatic vessels Testicle and epididymis, there is invasion of venous and lymphatic vessels Tumor invades the cord Tumor invades the tunica albuginea |
| Retroperitoneal lymph nodes | |
| N1 N2 N3 | >2 >5 cm |
| Distant metastases | |
| M1a M1b | Metastases to lymph nodes above the diaphragm and/or lungs Metastases to the liver, bones, brain |
Table 4.
Stage distribution according to TNM classification, 1997. [17]
| Stages | T | N | M | Markers |
| Stage 0 | pTis | NO | M.O. | SO, SX |
| Stage I | pT1-4 | NO | M.O. | SX |
| Stage IA | pT1 | NO | M.O. | SO |
| Stage IB | pT2 | NO | M.O. | SO |
| pT3 | NO | M.O. | SO | |
| pT4 | NO | M.O. | SO | |
| Stage IS | any pT/TX | NO | M.O. | S1-3 |
| Stage II | any pT/TX | N1-3 | M.O. | SX |
| Stage IIA | any pT/TX | N1 | M.O. | SO |
| any pT/TX | N1 | M.O. | S1 | |
| Stage IIB | any pT/TX | N2 | M.O. | SO |
| any pT/TX | N2 | M.O. | S1 | |
| Stage IIC | any pT/TX | N3 | M.O. | SO |
| any pT/TX | N3 | M.O. | S1 | |
| Stage III | any pT/TX | any N | M1, M1a | SX |
| Stage IIIA | any pT/TX | any N | M1, M1a | SO |
| any pT/TX | any N | M1, M1a | S1 | |
| Stage IIIB | any pT/TX | N1-3 | M.O. | S2 |
| any pT/TX | any N | M1, M1a | S2 | |
| Stage IIIC | any pT/TX | N1-3 | M.O. | S3 |
| any pT/TX | any N | M1, M1a | S3 | |
| any pT/TX | any N | M1b | any S |
Tumor markers - S
| LDH | CG (mIU/ml) | AFP (ng/ml) | ||
| SX | tumor markers were not determined or unknown | |||
| S0 | tumor markers are within normal limits | |||
| S1 | S2 | 1.5 – 10 x ULN* | 5000 — 50000 | 1000 — 10000 |
| S3 | >10 x ULN* | >50000 | >10000 | |
* ULN - upper limit of normal
Bibliography.
1. Scottish Intercollegiate Guidelines Network (SIGN). Guidelines on the management of adult testicular germ cell tumors. Royal College of Physicians of Edinburgh. Edinburgh, 1998.
2. Cancer Research Campaign. Factsheet 16 1998: Testicular Cancer - UK. London, CRC, 1998.
3. Cantwell BMJ, Macdonald I, Campbell S, Millward MJ, Roberts JT. Back pain delaying diagnosis of metastatic testicular tumors. Lancet 1989, ii, 739-740.
4. Rustin GJ, Vogelzang NJ, Sleiffer DT, Nisselbaum JN. Consensus statement on circulating tumor markers and staging patients with germ cell tumors. In: Newling DWW, Jones WG (eds): EORTC Genitourinary Group Monograph 7: Prostate and Testicular Cancer. Wiley-Liss, New York. Prog Clin Biol Res 1989; 357: 277-284.
5. Kennedy BJ. Testis Cancer: Clinical signs and symptoms. In: Vogelzang NJ, Scardino PT, Shipley WU, Coffey DS. (eds). Comprehensive Textbook of Genitourinary Oncology. (2nd Edition). Lippincott Williams and Wilkins, Philadelphia, 2000. pp. 877-879.
6. Thomas G, Jones W, van Oosterom A, Kawai T: Consensus statement on the investigation and management of testicular seminoma 1989. In: Newling DWW, Jones WG (eds): EORTC Genitourinary Group Monograph 7: Prostate and Testicular Cancer. Wiley-Liss, New York. Prog Clin Biol Res 1989; 357: 285 – 294.
7. Jones WG, Appleyard I. Delay in diagnosing testicular tumors. Br Med J 1985, 290:1550.
8. Thornhill JA, Fennelley JJ, Kelly DG, Walsh A, Fitzpatrick JM. Patients delay in the presentation of testis cancer in Ireland. Br J Urol 1987, 59:447.
9. Medical Research Council Working Party on Testicular Tumors. Prognostic factors in advanced non-seminomatous germ-cell testicular tumors: results of a multicentre study. Lancet 1985, i: 8-12.
10. Chilvers C, Saunders M Bliss J, Nicholls J, Horwich A. Influence of delay on prognosis in testicular teratoma. Br J Cancer 1989, 59:126-128.
11. Jones WG. Testicular cancer. Br Med J 1987, 295:1488.
12. Stoter G, Sylvester R, Sleijfer DT, et al: Multivariate analysis of prognostic factors in patients with disseminated nonseminomatous testicular cancer: Results from an EORTC multiinstitutional phase III study. Cancer Res 1987; 47: 2714 -2718.
13. Mead GM, Stenning SP: Prognostic factors in metastatic non-seminomatous germ cell tumors: the Medical Research Council studies. Eur Urol 1993;23:196-200.
14. Mead GM, Stenning SP, Parkinson MC et al: The Second Medical Research Council study of prognostic factors in nonseminomatous germ cell tumors. Medical Research Council Testicular Tumor Working Party. J Clin Oncol 1992; 10:85-94.
15. Peckham MJ: Investigation and staging: general aspects and staging classification; in Peckham M (ed): The management of Testicular Tumors. Edward Arnold, London, 1971, pp. 89 - 101. 19.
16. The International Germ Cell Cancer Collaborative Group: International Germ Cell Consensus classification: A prognostic factor-based staging system for metastatic germ cell cancers. J Clin Oncol 1997; 15: 594 – 603.
17. Sobin LH, Wittekind Ch, (eds): TNM classification of Malignant Tumors (UICC - International Union Against Cancer). Wiley-Liss, New York, 1997, pp 174 - 179
18. Azzopardi JG, Mostofi FK, Theiss EA. Lesions of tests observed in certain patients with widespread choriocarcinoma and related tumors. Am J Pathol 1961, 38:207-225.
19. Nichols CR. Mediastinal Germ Cell Tumors. In: Jones WG, Appleyard I, Harnden P, Joffe JK. (eds). Germ Cell Tumors IV. John Libbey, London, 1998. pp. 197-201
Diagnostics
To make a diagnosis, you must make an appointment with an andrologist or urologist. The examination consists of the following components:
- Examination, palpation of problem areas, interviewing the patient and taking an anamnesis.
- Ultrasound. The effectiveness of ultrasound examination in this case is very high.
- MRI or CT.
- Bone scintigraphy is necessary to detect metastases.
- Blood tests for tumor markers.
- Biopsy through inguinal access.
Interesting fact: one of the tumor markers is hCG. In women, the level of this substance increases during pregnancy. So some types of testicular cancer can be detected in the early stages using a pregnancy test.
Pain and increase in size of the scrotum
The main symptoms of testicular cancer are pain and enlargement of the scrotum.
Pain may appear in the scrotum area; it can be either aching or dull. Characteristic pain in the lower abdomen, which begins with varying strength, may not last long.
Sometimes heaviness appears in the lower abdomen. Pain is observed in the affected testicle. In addition, it is necessary to pay attention to uncharacteristic back pain. They can also be a symptom of developing testicular cancer.
When the cancer has already progressed, the scrotum swells and becomes asymmetrically enlarged.
Fatigue, weight loss, low-grade fever
Testicular cancer is characterized by signs such as a slight increase in body temperature, weakness, deterioration in emotional state, and depression. The patient's appetite decreases, dizziness may appear, and fatigue increases sharply. A feeling of fatigue appears even after minor exertion. Weight is decreasing. The temperature stays around 37.5, sharp jumps are usually not observed.
Treatment
Testicular cancer is treated in three ways:
- Surgical intervention. During the operation, the damaged testicle is removed, either just it or with adjacent lymph nodes.
- Chemotherapy. Usually prescribed after surgery.
- Radiation therapy is also prescribed after surgery. The specific program is selected individually.
When treating testicular cancer, there is a risk of developing infertility and/or impotence (often temporary phenomena). If a man still plans to become a father, he is recommended to freeze sperm using the cryopreservation method.
As for rehabilitation after surgery, the timing and duration vary from person to person. This also depends on the chemotherapy drugs chosen - on how a person tolerates the effects of such drugs. Clinical recommendations for testicular cancer are aimed at restoring a full life to the patient if possible.
Forecasts
If the symptoms and signs of testicular cancer were not ignored in the early stages, if you seek help in a timely manner, the five-year survival rate is 90-95%, that is, the prognosis is favorable. When treatment starts from stages 2-3, with proper treatment a survival rate of up to 85% can be achieved. The fourth stage has a less favorable prognosis - about 57%. But if the situation is neglected, the risks of death in the next three years are very high.
Causes of testicular cancer
The leading cause of gonadal tumors in men has not been determined.
A significant risk factor for the development of a malignant neoplasm is cryptorchidism - undescended testicles into the scrotum. With one undescended testicle, the risk of cancer increases 5 times, with bilateral cryptorchidism - 10 times. At the same time, the risk of developing tumors exists both when the testicle is left in the abdominal cavity and when it is brought down into the scrotum.
Sometimes testicular cancer develops from a teratoma - a tumor that begins during fetal development under the influence of maternal hormones - estrogens. Severe toxicosis of pregnant women and taking medications containing estrogens are considered risk factors.
Other causes that can lead to the development of testicular cancer include:
- atrophy of the glands, which occurs with cryptorchidism, mumps, testicular trauma;
- endocrine diseases – gynecomastia, hypogonadism;
- genetic pathologies – Klinefelter syndrome;
- HIV;
- radiation, exposure to chemicals.
Reasons that do not directly affect the development of pathology, but increase the risk of its occurrence, include hereditary predisposition, bad habits, low physical activity, and constant overheating of the testicles.
Prevention
To reduce the risk of developing testicular cancer, you must adhere to the following preventive measures:
- Regularly (at least once a month) conduct a self-examination of the scrotum and testicles for various lumps, formations, changes in size, etc.
- If any incomprehensible changes occur, seek advice from a urologist or andrologist.
- Lead a healthy lifestyle: stop smoking, alcohol, spend enough time on the move, eat healthy food.
- Avoid overheating the scrotum, as well as wearing too tight, rubbing clothes.
- Avoid various injuries to the genital organs. If an injury does occur, be sure to see an andrologist.
Paying attention to your own health will help you avoid serious consequences or detect testicular cancer at the very early stage, which will significantly increase your chances of recovery.
Psychological rehabilitation
Removal of a testicle is a powerful psychological trauma for a man. Even despite a favorable prognosis, recovery from a life-threatening disease, preservation of erection and sexual desire, and normal ability to reproduce, many men feel inferior due to the presence of one testicle in the scrotum. Fortunately, today this problem can be easily solved by implanting a silicone testicular prosthesis into the scrotum. The appearance of the scrotum after implantation and the prosthesis itself are completely indistinguishable to the touch from the real organ.
Why is it worth coming to Israel for testicular cancer treatment at Soroka MC?
The fight against cancerous tumors in an Israeli clinic is carried out through a combination of modern, most effective techniques. Complex treatment includes surgery followed by prosthetics of a removed organ, chemotherapy, radiation therapy, and each patient undergoes treatment according to a program developed personally for him.
When developing a personal treatment program, not only the stage, but also the type of tumor is taken into account. If the neoplasm is germinogenic, then treatment is carried out using primary irradiation.
Treatment of testicular cancer without removal
Early-stage nonseminoma tumors measuring no larger than 3 cm are treated with prophylactic chemotherapy or radiation therapy. The number of courses of therapy depends on the size of the tumor. Before starting treatment, patients are always offered to preserve sperm.
If, despite the therapy, the tumor continues to grow, then the combination of drugs is changed. In this case, an increase in the tumor to a size of more than 3 cm is an indication for surgical intervention.
How do cancer and malignant tumors develop?
The disease begins with the appearance of just one altered cell in the body. It is formed due to various health problems or hereditary characteristics, multiplies and gradually forms a tumor that grows and grows into the surrounding tissues. Our immunity copes with most of these cells - it identifies and destroys them, but some still manage to survive. In addition, they have one dangerous property - they enter the circulatory or lymphatic system. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking waste from them. In the lymph nodes, which act as “filters,” dangerous substances are neutralized and removed from the body. systems, and with their help spread throughout the body. After which they are fixed in its various areas and create metastases in them - additional neoplasms.
Reviews about the treatment of testicular cancer in Israel at Soroka MC
Dmitry, Omsk
“Four years ago I was diagnosed with testicular cancer. I immediately went to a private Moscow clinic to undergo a full examination. Based on the results of the examination, the doctors made a verdict - it is necessary to remove both testicles, and then undergo radiation and chemotherapy. It is possible that out of desperation I would have agreed to such treatment, but my friends suggested that I take advantage of the opportunity to get advice from foreign specialists. I turned to the doctors of the Israeli Soroka clinic for help and a week later I went to this clinic for treatment. It turned out that for treatment it is necessary to remove only one testicle and undergo several courses of chemotherapy. I am 100% satisfied with the treatment at Soroka MC, I am very glad that I turned to the specialists of this particular clinic.”
Cost of treatment for testicular cancer in Israel
The cost depends on the stage of the tumor, the complexity of the techniques used, the duration of hospitalization and other pricing factors.
Compared to prices in clinics in different countries, prices for treatment in Israel are the most affordable:
| Consultation with a urological surgeon | 573$ |
| Blood tests | from 23$ |
| MRI, PET-CT | from $1495 |
| Ultrasonography | 487$ |
| Orchiectomy, incl. hospitalization 1 day | 4896$ |
| Non-surgical treatment | from 1029$ |