How does pathology manifest itself?
Initially, the pathology is asymptomatic. The first signs of pathology may appear several months or even years after infection.
In newborns, congenital infection can be recognized by the following signs:
- yellowness of the skin;
- decreased platelet count;
- maculopapular skin rash.
The incubation period of the disease lasts about 2-3 weeks. During this time, most patients produce antibodies - specific substances aimed at combating the pathogen.
Acute toxoplasmosis resembles damage to the brain and its membranes. There is a headache, nausea, general weakness, convulsions are possible, tension in the muscles of the back of the head appears and the patient cannot bend the neck. Next, the optic nerve is damaged and vision deteriorates.
After this, myocarditis may occur. This is an inflammation of the muscle tissue of the heart. The organ ceases to perform its function normally, acute pain in the chest, interruptions in functioning, and rhythm disturbances are observed. The person feels weak and may lose consciousness. The danger of myocarditis is that those tissues that were inflamed can be replaced by scar matter. The condition is called cardiosclerosis and is an irreversible process.
Damage to the digestive organs is accompanied by dry mouth, dull pain in the abdomen, bloating, and impaired passage of gases from the intestines. Appetite decreases, stool may be disrupted.
The disease affects the functioning of the endocrine glands. This is reflected in disruption of the menstrual cycle, in men sexual function decreases, and the functioning of the pancreas is disrupted. A dangerous complication of the disease is recurrent miscarriage, which can remain with a woman for a long time.
Eye complications include uveitis, chorioretinitis, and myopia.
Changes such as muscle pain are observed in the musculoskeletal system. Particularly disturbing is the lower leg, thigh, lower back, neck and arm muscles. The pain occurs so sharply and acutely that the patient stops moving for some time.
Common symptoms include headache, high fever, general weakness, and chills. There is a reactive enlargement of the liver and spleen, the lymph nodes become inflamed, joints and muscles hurt.
The chronic course is accompanied by a less intense clinical picture and may be asymptomatic. If the temperature rises, it is only slightly. You are worried about a dull headache, weakness, memory and mental activity may be impaired.
With an exacerbation of the chronic process, chills and lymphadenopathy are troubling. Complications affect the nervous system and vision. Against the background of toxoplasmosis, the body may be affected by other infections.
As we can see, the disease either has no symptoms, which makes it impossible to make a timely diagnosis, or has so many different signs that it is difficult to make a differential diagnosis.
How to get rid
The treatment method for toxoplasmosis is selected depending on the form and course of the disease, as well as the presence of damage to internal organs. As a rule, the patient is prescribed antiparasitic drugs - most often chloridine, which is combined with sulfonamide drugs that enhance its effect. During pregnancy, spiramycin is often prescribed.
Usually the drugs are taken in three courses lasting from 5 to 10 days, repeated at weekly intervals. To eliminate the cause of toxoplasmosis in the chronic form, these drugs are not enough; additional immunotherapy is necessary using intradermal injections of toxoplasmin. At the same time, anti-allergy medications, courses of vitamins and immune stimulants are prescribed.
If the brain, visual organs and internal organs are damaged, appropriate therapy is prescribed.
Screening for toxoplasmosis during pregnancy
If during pregnancy a pregnant woman develops symptoms that may indicate the development of acute toxoplasmosis, it is necessary to establish the level of specific immunoglobulins using serological methods.
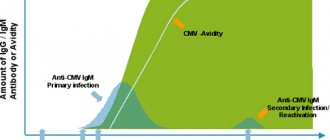
The enzyme-linked immunosorbent assay (ELISA) is best suited to detect the acute stage of the disease. It most accurately shows the concentration of IgM, an increase in the level of which indicates ongoing or recently present acute toxoplasmosis.
Determining IgG levels is less informative since these antibodies persist long after infection and indicate carriage rather than recent infection or exacerbation. Women who have been infected with toxoplasma before pregnancy are insured against infection of the fetus and are not at risk.
It is also important to obtain an immunological picture over time, for which specific tests are carried out at least once every 2 weeks. Studying the dynamics of changes in antibody titers allows us to establish a diagnosis with greater accuracy.
It should be taken into account that the serological picture indicating infection with Toxoplasma is not a 100% indication for termination of pregnancy. In this case, additional tests will be required by taking fetal blood from the umbilical cord and samples of amniotic fluid by puncture.
Examination of newborns and young children
Aimed at early detection of the pathogen, before the onset of the acute phase of congenital toxoplasmosis and the development of severe complications. Prescribed when there is a suspicion of Toxoplasma infection, includes the following tests:
- Isolation of the parasite by inoculating material from the placenta and umbilical cord into living mice.
- Carrying out PCR analysis of amniotic and lumbar fluids.
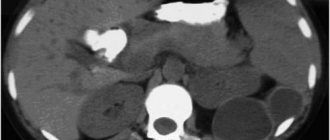
- Computed tomography or MRI of the head. Allows you to identify specific changes in the brain, for example, hydrocephalus, at an early stage.
Serological techniques are also used, but they provide only additional information. The newborn’s immune system is not active enough and is often unable to produce a sufficiently high titer of specific antibodies.
Examination in Medart
At the Medart Medical Center, a full range of serological tests are performed to detect toxoplasma in the patient’s body. An immunological test to identify specific immunoglobulins is part of comprehensive STD tests intended for couples planning to have a child. It is possible to take blood and other biological fluids to determine the presence of toxoplasma and clarify the clinical picture of the disease.
High-precision modern equipment allows you to obtain accurate research results in the shortest possible time.
Advantages of Medart Medical Center:
- Qualified specialists.
- The ability to quickly obtain accurate research results.
- Affordable price.
The medical center provides a full range of services, from preliminary appointments and consultations to establishing and clarifying the diagnosis and prescribing effective treatment regimens and prevention of toxoplasmosis and other diseases.
Differential diagnosis
It is carried out with diseases whose symptoms are similar to acute and chronic forms of toxoplasma infection. These include:
- Infectious mononuclease.
- Mycoplasmosis.
- Chlamydia.
- Cytomegaly.
- Tuberculosis.
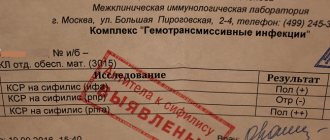
It is also necessary to exclude oncological pathologies and systemic diseases (rheumatism, lymphogranulomatosis). The final diagnosis is established after receiving the results of specific serological tests and PCR. There are many laboratory methods for detecting specific antibodies to Toxoplasma. These include:
- ELISA. Linked immunosorbent assay.
- RNIF. Indirect immunofluorescence reaction. Becomes positive from the first week of the disease. High antibody titers can last up to 15 years.
- RSK. Complement fixation reaction. It becomes positive from the 10-14th day of disease development and persists for 2-3 years.
Congenital toxoplasmosis occurring during pregnancy
Occurs when the parasite penetrates the placental barrier and infects the fetus. In most cases, it occurs during primary infection during pregnancy, less often - during relapse of toxoplasmosis associated with decreased immunity. The main risk group is women who were not infected with toxoplasma before pregnancy. If, as a result of contact with the pathogen, the disease manifests itself during pregnancy, the likelihood of developing congenital toxoplasmosis is quite high.
The survival rate of children with intrauterine infection depends on the period at which it occurred:
- If infected in the first trimester, the chance of fetal survival is 15%
- On the second – 30%.
- On the third – 60%
Even if pregnancy is successfully completed, an extremely high degree of development of congenital pathologies and congenital toxoplasmosis remains. The disease is severe, especially if infection occurs in the early stages. A characteristic tetrad of pathologies develops:
- Hydrocephalus.
- Bilateral retinochoroiditis.
- Delayed psychophysical development.
- Cerebral calcifications.
The prognosis for congenital toxoplasmosis is unfavorable; in most cases, the disease ends in the death of the newborn or severe disability. Even if, after intrauterine infection, an acute clinical picture does not arise, such children are at risk of developing:
- Mental deficiency.
- Epilepsy.
It is possible to develop many other pathologies that appear months and years after birth. For this reason, an acute form of toxoplasmosis that occurs during pregnancy is an indication for abortion even in the later stages. During pregnancy, it is necessary to undergo a lot of tests that help identify the presence of not only toxoplasmosis, but also CMV infection.
Indications for examination
Analysis is most often prescribed in two cases:
- When planning pregnancy as part of a standard laboratory diagnostic package for TORCH infection.
- If you suspect toxoplasmosis and have certain symptoms.
Laboratory diagnostics are also used to identify symptoms of acute toxoplasmosis in adults or children.
In general medical practice, this test is prescribed if patients exhibit specific symptoms (visual impairment, seizures), as well as for HIV-infected patients.
Pathogens of the disease, its sources
The most dangerous is intrauterine infection, which often ends in miscarriage or severe congenital pathologies. For this reason, testing for toxoplasmosis must be carried out in preparation for pregnancy and bearing a child.
According to statistics, toxoplasma is found in 25-80% of the world's population. In some regions, the infection rate reaches 95%.
Toxoplasma is an intracellular parasitic organism that can exist in three forms:
- Tachyozoites. They have a crescent shape and a size of 2-4 microns. A characteristic feature is that with special staining (Romanovsky-Giemsa), the nucleus becomes red, and the cytoplasm becomes blue-gray. In this form, the parasite penetrates the cells of the immune system (macrophages, phagocytes), in which it quickly multiplies. After cell death, tachyozoites are released and infect healthy macrophages.
- Bradiozoites (pseudocysts). This is a protective form of Toxoplasma, in which most of the life activity of the pathogen occurs during a normal immune reaction on the part of the infected organism. The shape of the bradiozoite cell is elongated, the nucleus is displaced towards one of the ends. Toxoplasma in this form often forms tissue pseudocysts consisting of many parasitic cells covered with a common protective membrane.
- Oocysts. This form of Toxoplasma is found only in the intestinal epithelial cells of the domestic cat and its wild relatives. Formed as a result of sexual reproduction of the parasite inside the cells of the animal. The immature oocysts are then released into the environment in feces. Given sufficient temperature and an influx of fresh oxygen, the oocysts mature within 2-7 days. After maturation is completed, oocysts become capable of infecting intermediate hosts of Toxoplasma, including humans.
The main source of infection is representatives of the cat family, the overwhelming majority being domestic cats. The mechanism of transmission of the parasite is fecal-oral. Implemented through:
- Consumption of insufficiently thermally processed meat products (especially pork and lamb).
- Through poorly washed vegetables, herbs, fruits.
- Failure to comply with personal hygiene rules (unwashed hands).
Rarely, direct infection with Toxoplasma through microdamage to the skin is possible. The parasite is rarely transmitted from mother to child. On average, one infection per 2-3.5 thousand pregnant women. It is most likely that the fetus will become infected with Toxoplasma if during pregnancy the pregnant woman’s body encounters the parasite for the first time.
Susceptibility to Toxoplasma is extremely high; single oocysts are sufficient for infection. Young people are most susceptible; in older people (after 60 years), the parasite is detected much less frequently.
Examination of patients with HIV infection
Diagnosis consists of regular monitoring of immunoglobulin G titers using serological methods. Titration of immunoglobulin M is not informative since in most HIV-positive people the level of antibodies of this group is extremely variable.
Direct detection of the pathogen by microscopy of tissue samples or infection of laboratory animals is usually not necessary. The diagnosis can be established quite accurately through serological diagnosis and the presence of a specific clinical picture of toxoplasmosis. In HIV-positive patients it is more pronounced, which greatly simplifies the diagnosis.