Thomas W. Kraus, visceral surgical oncologist
Since 2005, Professor Kraus has been working as the chief physician of the Department of General and Visceral Surgery at the Nordwest Clinic in Frankfurt am Main.
Read more about the specialist →
There are several types of cystic changes in the pancreas, which are usually discovered by chance. In 70-90% of cases we are talking about so-called pseudocysts (fluid-filled voids), which can develop after acute or chronic inflammation. In addition to false ones, in 10-15% of cases pancreatic cysts are cystic edema of the gland. In this case, benign, malignant and borderline neoplasms are distinguished. In the latter case, we are talking about the borderline quality of the tumor between benign and malignant. During histological examination they are considered as malignant prestages of the tumor.
True benign pancreatic cysts are divided into the following types:
- serous cystadenomas;
- mucinous cystadenomas;
- intraductal papillary mucinous neoplasia.
Since all of these tumors have the potential for malignant change, surgical treatment is usually indicated.
Symptoms of the disease
Small pancreatic cysts usually have no symptoms. If they occur, patients most often complain of uncharacteristic, sometimes girdling pain in the epigastric region. Later, lack of appetite, weight loss, nausea and fatigue appear. If the tumor presses on the bile duct on its way from the liver to the duodenum, jaundice may occur. However, all these symptoms are rather nonspecific, and this makes early diagnosis much more difficult. To identify pancreatic cysts without relying on the primary signs of their manifestation, you need to regularly undergo diagnostics of your health. In Germany, you can do this with the help of a special check-up program developed by the Nordwest Clinic for its patients.
Etiology of retroperitoneal cysts
This type of cyst is considered quite rare and at the initial stage practically does not manifest itself, which determines its danger: as it develops, suppuration develops, pressure on the internal organs and the risk of rupture of the membrane increases. The above poses a real threat to the patient’s health. The initiating factors for the development of cysts in the retroperitoneal space are as follows:
- traumatic injuries to the abdominal area;
- hereditary predisposition;
- congenital anomalies of the abdominal organs;
- parasitic lesions;
- effects of a chemical nature on the peritoneal area;
- hemorrhages and inflammatory processes of internal organs.
Diagnosis of cystic formations
After a detailed study of the patient's history and physical examination, an instrumental examination is performed. Typically, to identify a pancreatic cyst, thin-layer computed tomography (CT) of the abdomen is prescribed, as well as ERCP (endoscopic retrograde cholangiopancreatography), which visualizes the bile and pancreatic ducts. In this case, it is possible to perform an endoscopic ultrasound examination (ultrasound) and, in some cases, it is necessary to examine the surrounding vessels, for which magnetic resonance imaging (MRI) is performed.
Preoperative biopsy for resectable tumors is not performed to avoid tumor transfer.
Risk of complications from retroperitoneal cysts
As already mentioned, the danger of this type of cyst is that at the initial stage of development they are practically not manifested by anything. The patient does not seek professional medical help, and in the meantime the tumor grows and after a short period of time poses a danger to his health and even life.
The fact is that large-diameter cysts put pressure on internal tissues and organs. Their most dangerous complication is spontaneous opening of the capsule, which can occur due to a blow to the stomach or due to physical exertion. In this case, the serous or purulent contents of the cyst enter the abdominal cavity and cause intoxication, which requires urgent hospitalization.
Therapeutic measures
Depending on the location and size of the tumor, various surgical techniques are used. The goal is always to completely remove the pancreatic cyst during surgery within healthy tissue (R0). Therefore, during surgery, a cytological examination of the tissue is carried out in order, if necessary, to expand its volume during the operation and completely remove the tumor.
If the tumor is localized in the area of the head of the pancreas, it is resected while preserving the pylorus or Whipple surgery (pancreaticoduodenectomy). If the cyst is localized in the tail of the pancreas, distal resection of the gland is performed, if necessary, with removal of the spleen. If the tumor spreads to both parts and is malignant, in rare cases, complete removal of the pancreas may be indicated.
Hygroma
Arthritis
21738 December 17
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Hygroma (articular hernia, synovial cyst, ganglion): causes, symptoms, diagnosis and treatment methods.
Definition
Hygroma is a benign cystic tumor that is formed from the superficial membranes of the joint and is a clearly demarcated capsule filled with a viscous serous fluid. The contents of the cyst are liquid with mucus, proteins and fibrin, which determines its jelly-like state. The size of the formation ranges from a small pea to the size of a walnut and even larger. The shape of the formation is most often round or elongated. The base of the hygroma is tightly connected to the underlying tissues, and the remaining surfaces are mobile and not fused to the skin and subcutaneous tissue. The skin above the hygroma moves freely.
Hygroma is an organ-specific cyst that forms only in the immediate vicinity of the joint and is not found in other organs and tissues.
Causes of hygroma
It is assumed that the root cause of the development of such a cyst is the degeneration of connective tissue cells. In this case, there are two types of cells: spindle-shaped - they form a capsule, spherical - they are filled with liquid, which, when the walls of the tendon sheath are damaged, spills into the intercellular space of nearby tissues.
The degeneration of connective tissue cells is facilitated by injuries or stretching of tendons, inflammation of the joint capsule (bursitis, synovitis, arthritis, tenosynovitis, etc.).
In addition, the formation of hygroma can be explained by hereditary predisposition, and can also be a consequence of improperly selected shoes.
Hygromas are localized in the area of the fingers, in the area of the foot, knee or elbow joints, but the most common location (about 70%) is the area of the wrist joint. The reason for this “selectivity” is the daily monotonous physical load on the mentioned joints and tendons among representatives of certain professions. The risk group includes:
- athletes (tennis players, golfers, table tennis, badminton),
- musicians (pianists, violinists, cellists),
- programmers,
- typists,
- massage therapists, seamstresses, embroiderers, etc.
Hygroma is common among both children and adults, but is most often seen in people aged 20–45 years. This cystic formation cannot disappear on its own, without therapeutic measures. However, it should be noted that hygromas never degenerate into cancer, so the prognosis is very favorable.
Classification of the disease
Hygromas can be single-chamber or multi-chamber. The latter appear as a result of several effusions of serous fluid and are often localized in one or several areas.
According to their structure, hygromas are divided into the following types:
- isolated hygroma - the spilled liquid is in a confined space and does not have a connecting “bed” with the tendon sheath;
- anastomosis - a new cavity is formed, the fluid of which moves freely from it to the tendon sheath and back;
- valve - the serous fluid completely moves to a new place, since a barrier formed in the tissues, called a valve, prevents it from returning to the empty vagina.
Symptoms of gyroma
In the vast majority of cases, hygroma develops slowly, is single, has a diameter of no more than 3 centimeters, does not cause pain or discomfort, so it is noticed when it reaches a fairly impressive size. The early stage of the disease is characterized by the formation of a small cyst that rises above the surface of the skin. In approximately 35% of cases, hygroma is asymptomatic. Quite rarely, when a cyst is located under a ligament, it can go unnoticed for a long time. In such cases, patients consult a doctor because of pain and discomfort when bending the joint.
If the hygroma begins to compress the nerve endings, the patient may experience pain. A dull pain spreads to surrounding tissues and intensifies after intense exercise.
Depending on the location, there are both very soft, elastic, and hard tumor-like formations, resembling bone or cartilage in density.
The skin over the hygroma may remain unchanged or become rough, acquire a reddish tint and peel off. After active movements, the hygroma can increase slightly, but at rest it returns to its original size.
Diagnosis of hygroma
Usually the diagnosis is made on the basis of anamnesis and characteristic clinical manifestations.
An ultrasound examination makes it possible not only to see the cyst, but also to evaluate its structure and determine whether there are blood vessels in the wall of the hygroma.
Postoperative period
After the operation, the patient is monitored in the intensive care unit for several days. From the first day it is important to mobilize the patient and breathing exercises to prevent pneumonia. Particular attention is paid to blood sugar levels in order to promptly recognize possible diabetes mellitus caused by such operations. Gradual restoration of nutrition, therapeutic exercises, and respiratory therapy are carried out. When a large part of the pancreas is removed, replacement therapy for enzymes produced by the pancreas is started. As a rule, the patient is discharged 10-14 days after surgery.
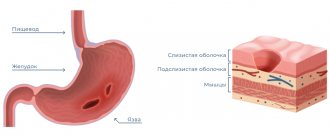
Pathogenesis
The development of pancreatic cysts occurs under the influence of provoking factors, resulting in discomplexation of pancreatocytes in the pancreas with the development of small diffuse necrosis of acinar (secreting) cells. As a consequence, there is a violation of secretion into the lumen of the ducts and parapedesis of secretory granules in the interstitium. Destroyed cells promote interstitial/intracellular activation of trypsin, which activates pancreatic hydrolytic/proteolytic enzymes, which in turn contribute to autoenzyme aggression and the development of foci of necrosis, which is manifested by regional rheological disorders and severe interstitial edema.
Resorption of pancreatic enzymes from the interstitium contributes to autolytic damage to blood vessels with the subsequent development of thrombohemorrhagic local syndrome.
The formation of fluid accumulations is based on the processes of lysis of foci of infiltration/necrosis. The formation of fluid accumulations is ensured mainly due to the exudative reaction of inflamed tissues and, to a lesser extent, due to pancreatic juice arriving due to a violation of the outflow of juice along the main pancreatic duct. As a result of a pronounced violation of capillary permeability, almost within 1–2 hours after the destruction of the acini, many mast cells/leukocytes appear in the tissues, actively secreting biologically active substances, which leads to the formation of a demarcation shaft around the focus of necrosis, consisting of leukocytes, fibrin, histeocytes, lymphoplasma cells components and nuclear detritus.
Activation of fibroblasts promotes the intensive formation of elements of connective tissue structures/collagen, which serve as the basis for the formation of a barrier, which subsequently becomes the base of the postnecrotic cyst capsule.
Cost of surgical treatment of pancreatic cysts in Germany
Before removing a tumor, it is important to undergo examination and receive clinical recommendations from the attending physician at the Nordwest clinic. Accurate adherence to the prescribed treatment regimen helps to avoid possible complications after removal of a pancreatic cyst and quickly return to your normal rhythm of life. Treatment in Germany will help you cope with the disease and eliminate as much as possible the consequences of its manifestation in the body. The best doctors who have repeatedly confirmed their high qualifications in practice work with the hospital’s patients. Prices for removal of pancreatic cysts can be clarified upon your first visit. The cost of all treatment includes a consultation with a doctor, diagnostic tests, surgery, as well as the rehabilitation period after.
Acute pancreatitis.
Acute pancreatitis is an acute inflammation of the pancreas.
Acute pancreatitis usually appears against the background of a person’s abuse of alcoholic beverages and previous alcohol poisoning.
Acute pancreatitis can also be caused by:
- improper or poor quality nutrition (eating fatty, spicy foods, frequent overeating);
- urolithiasis – the presence of kidney stones;
- heredity;
- trauma to the pancreas: previous operations, injuries, mechanical damage;
- uncontrolled use of medications, antibiotics;
- endocrine diseases, hormonal disorders.
- infections and viruses.
Symptoms of acute pancreatitis in Nizhny Novgorod.
The main symptom of pancreatitis is acute pain in the epigastric region, hypochondrium (right and left). Over time, the pain begins to become encircling, affecting the back, lower and lateral areas of the abdomen.
Detection of acute pancreatitis in Nizhny Novgorod.
If you suspect the development of pancreatitis in the body, the gastroenterologist prescribes the following set of examinations:
- a general blood test, which allows you to find out about the presence of an inflammatory process;
- Ultrasound of the abdominal cavity, which allows you to see changes in the internal organs;
- a general urinalysis to detect amylase in the urine, the presence of which indicates the development of pancreatitis;
- FGDS.
Presence of pancreatic abscess
A localized collection of pus within or adjacent to the pancreas has traditionally been described as an infected pseudocyst, a condition requiring prompt incision and drainage. Recently, endoscopic drainage has been used in a group of patients at high surgical risk due to the presence of systemic complications of pancreatitis [35]. Important factors include adequate drainage, the need to relieve outflow obstruction, and diligent patient education and monitoring. We prefer the transmural approach to abscess drainage because... it allows for further drainage of the cystenterostomy channel, insertion of a nasogastric irrigation catheter and multiple stents to prevent complications associated with insufficient catheter function and residual contents.
Drainage options
In the past, when drainage became necessary due to complications or intractable symptoms associated with PC, surgical drainage remained the only treatment option. Currently, there are two more treatment options that have achieved increasing popularity: percutaneous and endoscopic drainage. The remaining controversy is which of these methods should be offered to the patient as the initial type of therapy. Currently, there are no randomized comparative studies of these two methods and doctors use the one they are better at. The disadvantage of percutaneous drainage is the long stay of the catheter and the possible formation of an external fistula.
Internal surgical drainage.
Most surgeons, if possible, use the internal drainage technique, the technique of which depends on the location of the pseudocyst:
- Cysto-gastro or duodenostomy when a cyst is fused with the stomach or duodenum.
- Cystojejunostomy can be used for other anatomical variants.
- The PCs of the tail of the pancreas can be removed during pancreatic resection; in these conditions, papilosphincterotomy is often necessary.
The reported complication rate of internal drainage is approximately 15% with a mortality rate of less than 5%. The postoperative recurrence rate is about 10% [22–26]. When there is obstruction of the main pancreatic duct below the level of the anastomosis, some surgeons prefer PC resection rather than internal drainage in an attempt to minimize recurrence rates.
External surgical drainage
may be necessary if it is impossible to create an internal anastomosis. External pancreatic fistulas are a common outcome of this approach [27].
Percutaneous drainage with a catheter.
Percutaneous catheter drainage is as effective as surgical drainage in draining and closing both sterile and infected cysts [28–30].
It is necessary to maintain patency of the catheter by careful irrigation. The catheter is left in place until the discharge level drops to 5-10 ml. in a day. In one study of 52 patients, the average drainage time was 42 days [28]. If such a decrease in the level of discharge does not occur, then the administration of octreotide (50-200 mg subcutaneously, every 8 hours) may be useful. A control CT scan should be performed when the amount of discharge decreases to ensure that the catheter has not dislodged from the PC cavity. The main complication of this procedure is catheter infection, which occurred in half of the patients in one study [28]. It is unknown whether obstruction of the main pancreatic duct should deter percutaneous drainage. Endoscopic approach.
Multiple reports confirm the high success rate of endoscopic cysto-gastro (ECG) and cysto-duodenostomy (ECD). ECD is the procedure of choice due to its higher safety, easier achievement of a perpendicular approach to the cyst during drainage, and greater involvement of the duodenum than the stomach in most cases of PC. The resolution level of PC during endoscopic treatment varies from 65 to 89%. The main complications of endoscopic drainage are bleeding (which, due to its severity, requires surgical treatment in up to 5% of cases), retroperitoneal perforation, infection and failure to achieve resolution of PC. There is virtually no mortality associated with this procedure, with a recurrence rate of 6-18%. The incidence of perforation or bleeding can be minimized by detecting the PC prior to endoscopic puncture. We prefer detection of PC by endoscopic puncture, although the increasing popularity of endoscopic ultrasound may make this technique a viable alternative.
Recommended approach
Currently, we recommend active tactics in patients with pancreatitis arising as a complication of chronic or acute pancreatitis with the presence of symptoms and duration of pancreatitis of at least 4 weeks. We perform ERCP when we believe that the patient is a candidate for attempting endoscopic drainage. During endoscopy, it is necessary to exclude portal hypertension and obstructive gastric emptying disorders. RCCP is performed to detect signs of compression of the biliary tree, especially if liver parameters are elevated. Pancreatography is necessary in all patients to identify underlying pancreatic duct obstruction. Unexpected pancreatic duct strictures and calculi are often detected, and a stricture caused by a malignant tumor may even occur. Because Endoscopic drainage can be performed either by transmural puncture or transpapillary stent placement; a pancreatogram is very important for choosing between these two options. Endoscopic ultrasound may be useful in the differential diagnosis of cystic lesions of the pancreas and drainage of the pancreas, although it is not routinely used. Patients with large, persistent or enlarging pancreatic ducts often exhibit severe pancreatic duct damage, which determines the need and type of treatment used [10]. In our experience, pancreatic duct obstructions and complete strictures are common in this group of patients and do not resolve after resolution of the pseudocysts. In contrast, leaks from peripheral branches close after endoscopic treatment leading to resolution of the cyst.
We recommend:
- The role of intraluminal endoscopic interventions in the complex treatment of chronic pancreatitis and its complications
- Diagnostic RCP. Execution technique
- Diagnosis and treatment of pancreatic pseudocysts
- Endoscopy for primary sclerosing cholangitis: clinical recommendations of the European Society
- Recommendations for surgical treatment of chronic pancreatitis 2016
- Stenting and ERCP under ultrasound
- Draft national clinical guidelines “Obstructive jaundice”
Articles on the topic - see the selection of articles at the bottom of the page
The role of endoscopic ultrasound
The popularity of endoscopic ultrasound in the diagnosis of pancreatic pseudocysts is currently growing due to the fact that this technique allows one to recognize the complex structure of the walls and contents of the pancreas. In combination with aspiration biopsy, it can help in the differential diagnosis of PC and cystic neoplasm [31]. The presence of well-differentiated septa, echogenic mucin, and masses indicates a cystic neoplasm requiring resection rather than drainage. As mentioned above, endoscopic ultrasound can help in choosing the site of pseudocyst puncture - to exclude the presence of large veins or arteries in the drainage area [32]. Thus, it is theoretically possible that this technique may have an advantage by reducing the risk of bleeding and perforation, although this has not been demonstrated in controlled studies.