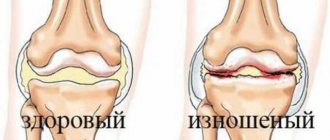
Gonarthrosis or arthrosis of the knee is not a disease of an inflammatory nature. This pathology is a progressive degenerative-dystrophic disorder in the functioning and structure of intra-articular cartilage tissue. The disease can progress. It has 4 stages of development. When stage 2 arthrosis of the knee joint occurs, the patient is still capable of independent movement, although there is a significant decrease in his activity. Let's look at the main causes of this disease and effective treatment methods.
Types of gonarthrosis 2 degrees
As joint activity decreases, the patient becomes irritable. The occurrence of severe painful sensations leads to a deterioration in the quality of life. The risk group includes people who are professionally involved in sports or ballet. The disease also develops in people whose work involves constant heavy lifting and prolonged standing. Office employees also suffer from gonarthrosis, which is associated with prolonged sitting.
Arthrosis of the knee joint stage 2 can be primary or secondary. Often, patients are diagnosed with a secondary form of pathology. In this case, the disease develops against the background of:
- previous knee injury;
- advanced forms of arthritis and some other pathological processes occurring in the body
- as a consequence of the progression of diseases of the endocrine system (diabetes, problems with the thyroid gland, etc.).
The primary form of knee arthrosis is characterized by the causeless appearance of a degenerative-dystrophic process in the cartilage tissue of the knee joint. This condition is observed in rare cases.
The joints are affected symmetrically, there is a complete absence of joint space. In turn, both primary and secondary forms of grade 2 gonarthrosis can affect not only one knee, but both at once (both right and left). If the cartilage tissue of only one knee joint is affected, orthopedists call this disease unilateral. If the knees of both lower extremities are affected simultaneously, this is bilateral gonarthrosis.
Bilateral knee arthrosis of the 2nd degree is much more difficult for patients to endure, since serious deformation of the articular tissue is observed simultaneously in both legs. Based on etiological characteristics, this type of pathology is most often classified as idiopathic (primary) type. The same applies to the unilateral form of gonarthrosis; it is almost always secondary.
Regardless of the type of arthrosis of the knee joint, stage 2, conservative methods are used at the initial stage of treatment. If the desired result after the therapy is not available, surgical intervention is resorted to.
Non-surgical treatment has a positive effect only if stage 1-2 knee arthrosis is diagnosed. In some cases, at this stage, surgical intervention may be required.
It should be noted that the use of conservative methods cannot cure gonarthrosis completely (any arthrosis is an incurable disease). Non-surgical therapy is:
- competent prevention of subsequent destruction of cartilage tissue with properly selected medications and physical preparations;
- symptomatic relief from painful symptoms due to the use of painkillers;
- a means of maintaining muscle and ligamentous tissue by performing special gymnastic exercises. This helps to some extent to activate motor function.
The use of conservative technologies is advisable at an early stage of the disease. If the middle phase of arthrosis of the knee joint is diagnosed, such techniques become less effective, although in some cases they help improve the patient’s condition.
If the last phase of gonarthrosis is identified, non-surgical treatment methods become useless. The use of alternative medicine for therapeutic purposes in severe stage 2-3 gonarthrosis is ineffective. Without seeking specialized help, the disease will progress. In this case, destructive processes appear inside the knee cartilage.
If you do not consult a doctor in a timely manner and do not undergo appropriate treatment, this may even cause disability.
A person may be assigned a disabled group in the following cases:
- grade 2 arthrosis of the knee joint was diagnosed;
- the disease is accompanied by persistent and pronounced functional disorders;
- the disease is characterized by a rapidly progressing degenerative and dystrophic process in the cartilage tissue of the joint.
When the pathology reaches the last phase, the patient is in any case recognized as disabled. No gentle therapeutic techniques are used in such a situation. Treatment in this case consists of removing non-viable articular tissue, after which an artificial joint is installed.
With the help of endoprosthetics at an advanced stage of gonarthrosis, it is possible to restore lost locomotor-support functionality for a long time (for a period of 15 to 30 years).
Knee replacement for deforming gonarthrosis
Non-invasive or minimally invasive treatment that was not successful at stage 2 is pointless to use anymore. To effectively help the patient restore their quality of life, experts recommend undergoing high-tech arthroplasty. This surgical intervention allows in 95% of cases and above to achieve complete restoration of the limb’s functionality. Intraoperative and postoperative complications are minimal: negative phenomena practically do not occur with correctly performed intervention and impeccably organized rehabilitation.
Very often surgery is the only option.
The procedure for replacing a failed biological joint is the only real salvation for many patients with an incurable chronic pathogenesis. The productivity of such implantation has been reliably confirmed by multicenter clinical studies. According to many years of practical observations, with an artificial left-sided and/or right-sided analogue joint, the amplitude of movements is restored to full volume.
Simplified implant installation diagram.
A minimum of 15 years must pass before the next reinstallation of the prosthesis, although in most cases the non-native structure serves well on average for 20-25 years. We will once again emphasize that the main conditions for the long service life of a unique device that functions similarly to a healthy joint and a favorable prognosis are high-precision placement of an artificial prosthesis and high-quality postoperative rehabilitation of the patient.
Knee implant in mock-up.
The implanted product, which is placed instead of a destroyed knee joint, comes in various types, depending on the degenerative-dystrophic specifics. The most widely used types of endoprosthetic systems are:
- unicondylar prosthesis – the lateral or medial condyle of the tibia is subject to prosthetics;
- total implant with a movable platform - such models involve a complete replacement of articular surfaces (the most expensive, but considered the most physiological);
- linked endoprosthesis - used in situations where the ligamentous apparatus of the knee is additionally damaged (mechanical stabilizers in this device will play the role of ligaments).
The structure of knee prostheses follows the natural configuration of the joint or its individual part, which needs to be replaced due to irreversible changes that have occurred. Modern endoprostheses are made from ultra-technological metal alloys based on titanium, chromium, cobalt, molybdenum or high-strength ceramics.
A unicondylar implant made of black ceramic is subject to longer wear.
The implant model and attachment method are selected by the operating surgeon at the preoperative stage of preparation. Based on the type of fixation, innovative designs are:
- cement – bonded to the bone using medical cement;
- cementless – fixed by hammering;
- hybrid - one of the elements is placed on cement, the second is hammered into the bone using the “press fit” technique.
The surgery is performed under spinal (most often) or general anesthesia. The entire replacement process takes approximately 2 hours. The essence of the procedure is the resection of the deformed end elements of the articular bones, followed by the correct installation and rigid fixation of the endoprosthesis components. Immediately after prosthetics, they begin to implement a rehabilitation program, which provides for intensive prevention of all possible complications and high-quality development of the operated limb.
Symptoms and diagnosis
For stage 2 arthrosis of the knee joint, the clinical picture is more pronounced, although the symptoms are not yet critical. This degree of the disease is accompanied by the following symptoms:
- Regular painful manifestations in the knee area, but at this stage they do not yet become permanent. The pain starts to bother me in the morning, not every day. In addition, after about 15 minutes the discomfort goes away. At this stage, prolonged walking or intense physical activity is accompanied by the appearance of an unpleasant pain syndrome.
- Painful manifestations that often occur against the background of increased loads on the damaged area. To prevent them, the patient tries to reduce the load on the knee joint as much as possible. This is not recommended. Such actions can lead to atrophy of the muscle tissue surrounding the joint.
- A dull aching pain syndrome that occurs in damaged cartilage tissue of the knee joint under the influence of reduced atmospheric pressure. In medical practice, this phenomenon is called weather dependence, and such a condition does not have an exact definition. According to some doctors, when the pressure in the atmosphere decreases, this leads to an increase in the pressure of the intra-articular fluid. This condition leads to painful sensations.
- Crunching in the knees, characteristic of stage 2 gonarthrosis. In addition, as the pathology progresses, it intensifies.
Also, with stage 2 arthrosis of the knee joint, another characteristic sign is observed, but only a specialist can determine it on an x-ray. The space in the knee joint tissue narrows, and this process is accompanied by the formation of bone growths - osteophytes. On X-ray film they are visualized as tubercles.
At this stage of pathology progression, a certain deformation of the cartilage tissue in the joint occurs. For this reason, in some cases there is not complete, but partial flexion and extension of the injured limb. This is fraught with the appearance of pain.
Diagnostic measures for identifying stage 2 knee arthrosis consist of interviewing the patient, collecting anamnestic data, and also conducting some examinations. A differential diagnosis is also required, since the symptoms of the disease are similar to some diseases of the knee of inflammatory etiology.
Methods of treating the disease
Only an integrated approach to the treatment of grade 2 gonarthrosis is used. It is aimed at restoring range of motion, eliminating pain and morning swelling, and preventing the involvement of healthy tissues and joints in the degenerative process. Throughout therapy, patients must avoid fixed positions and prolonged standing.
Drugs
In the treatment of pathology, drugs from many clinical and pharmacological groups are used in various dosage forms. Outside of exacerbations, external agents are usually used - ointments, gels, balms. Taking tablets, capsules, and pills helps eliminate moderate pain characteristic of the subacute period. And during relapses, intramuscular, intra-articular, periarticular administration of injection solutions is practiced to relieve severe pain.
Anti-inflammatory drugs
NSAIDs quickly eliminate pain and inflammatory swelling, reduce local temperature with synovitis accompanying grade 2 gonarthrosis. Of the local remedies, gels and ointments Voltaren, Fastum, Indomethacin, Diclofenac, Artrosilene are especially in demand. In the form of tablets, patients are prescribed Ibuprofen, Ketorol, Nimesulide, Celecoxib, Etoricoxib. For intramuscular administration, Xefocam, Movalis, Ketorolac, Ortofen are used.
If NSAIDs are ineffective, glucocorticosteroids Diprospan, Triamcinolone, and Dexamethasone are included in treatment regimens. Hormonal agents in combination with anesthetics are intended for drug blockades.
Treatment with chondroprotectors
Chondroprotectors are drugs that improve metabolism in cartilage and bone tissues, stimulating their partial restoration. As the ingredients accumulate in the knee joint, the analgesic, anti-inflammatory, and decongestant effects of these drugs also appear. Frequently prescribed chondroprotectors include Artra, Structum, Chondroguard, Alflutop, Teraflex.
Painkillers
In addition to NSAIDs and glucocorticosteroids, muscle relaxants (Mydocalm, Sirdalud), which relax spasmodic muscles, can be used as painkillers. Outside of exacerbation, drugs are also used for local application with a warming, locally irritating, distracting effect. These are ointments and gels: Finalgon, Capsicam, Viprosal, Nayatoks, Apizartron.
Injections
In the form of injections, NSAIDs, muscle relaxants, glucocorticosteroids, and chondroprotectors are used for the treatment of grade 2 gonarthrosis. It is mandatory to prescribe medications with B vitamins - Milgamma, Combilipen. At the initial stage of therapy, injection solutions of Nicotinic acid and Pentoxifylline can be used to improve blood circulation in the knee joint.
Orthopedic treatment
In the acute and subacute period, elastic semi-rigid knee pads should be worn during the daytime to reduce stress on the joint. They are equipped with metal or plastic inserts (spirals, rings, plates) that reliably fix the knee, but do not hinder movement. For acute pain, it is advisable to use a cane while walking. During the remission stage, orthopedists recommend wearing soft warming knee pads made of sheep or camel wool.
Physiotherapy
To improve the blood supply to joint tissues with nutrients and increase the body's sensitivity to pharmacological drugs, patients are prescribed physiotherapeutic procedures. For grade 2 gonarthrosis, magnetic therapy, laser therapy, UHF therapy, applications with ozokerite or paraffin, and mud therapy are most effective.
Massage
In the treatment of pathology, classical, vacuum (cupping), acupuncture (acupressure), connective tissue massage is used. After 10-20 sessions, the severity of pain decreases, stiffness of movement, muscle spasms, crunching and clicking that accompany flexion and extension of the knee disappear.
Diet and nutrition rules
Orthopedists advise overweight patients to lose weight to reduce the load on the knee joints. In the diet, it is necessary to limit the consumption of foods high in fat and simple carbohydrates - sausages and confectionery products, baked goods, semi-finished products, smoked meats. They should be replaced with low-fat cheeses, cottage cheese, cereal porridges, fresh vegetables, fruits, and berries.
Physiotherapy
After the acute pain has been relieved, the physical therapy doctor will create an individual set of exercises. It necessarily takes into account the patient’s physical fitness, the severity of symptoms, and the cause of the development of gonarthrosis. Daily physical therapy exercises help strengthen muscles and restore the usual range of movements.
Rules for performing exercises
A physical therapy doctor is present at the first training sessions, monitors the execution of exercises, and advises how to dose the load correctly. They should be increased gradually for optimal muscle adaptation. It is advisable to start performing technically complex exercises after 2-3 weeks of regular training.
Exercises by Evdokimenko
Dr. Evdokimenko has developed a method for treating grade 2 gonarthrosis using smooth, slow movements that promote the rapid formation of the muscle corset of the knee. What exercises are most effective:
- sit on a chair, alternately raise your legs slightly bent at the knees, lingering at the point of maximum muscle tension for 10-15 seconds;
- lie on your back, at the same time raise your legs 15-20 cm from the floor, spread them apart;
- stand up straight, lean on the back of a chair, roll from heels to toes, trying to hold each position for 10 seconds.
Each exercise must be performed 7-10 times. The workout should be stopped if pain occurs in the knee.
Popov's exercises
Rehabilitation doctor Popov is the author of a method for restoring all knee functions by strengthening the muscles and ligamentous-tendon apparatus. The complex he developed includes the following exercises:
- lie on your back, slowly pull your knees towards your body, clasping them with your hands;
- lying on your back, make circular rotations with your knees, simulating riding a bicycle;
- lie on your stomach, stretch your arms along your body, alternately raise and lower your shins.
The number of repetitions is 10-15. You need to perform the exercises on a gymnastic mat or soft carpet.
Endoprosthetics
Surgical treatment of grade 2 gonarthrosis is performed quite rarely. Indications for it include the ineffectiveness of conservative therapy for several months, rapid progression of the pathology, and persistent pain. When choosing a surgical technique, preference is always given to endoprosthetics. Replacing a worn knee joint with an endoprosthesis allows the patient to return to an active lifestyle after 3-6 months of rehabilitation.
Folk remedies and recipes
Ointments, compresses, herbal teas, alcohol and oil tinctures are used during the remission stage, when the main treatment has already been carried out. Folk remedies are used to eliminate mild pain that occasionally occurs after increased stress on the knee.
| Folk remedy for the treatment of grade 2 gonarthrosis | Cooking method |
| Pain relieving ointment | Grind a teaspoon of alcohol tincture of red pepper with 20 g of thick honey in a mortar. Add a couple of drops of thyme and mint essential oils, a tablespoon of flaxseed oil. Introduce 100 g of medical Vaseline in small portions |
| Decongestant compress | Dissolve a tablespoon of sea salt in a glass of hot water. Cool the resulting dilution and soak a bandage folded in several layers in it. Squeeze it lightly and apply it to your knee for an hour. |
Carrying out an external inspection
Initially, the patient should be examined by an orthopedist. During a visual examination, the doctor determines:
- roughened contours of bone tissue;
- deformed joint;
- curved limb axis.
When moving transversely, the kneecap crunches and a click may be heard. During a palpation examination, the doctor can detect zones in and around the gap of the knee joint that, when pressed, respond with the appearance of pain.
Functional tests are required to assess motor activity and muscle strength.
Stage 2 arthrosis of the knee is often accompanied by synovitis (an inflammatory process in the synovial membranes). This condition is characterized by the occurrence of swelling in combination with hyperemia of the skin. There is a smoothing of the contours of the knee, the formation of a rounded seal. If you press on it, you can feel the fluid moving in the middle of the joint. This phenomenon is called fluctuation.
How the disease develops
Initially, gonarthrosis affects the cartilaginous layer of the knee joint. It becomes thin, fragile, and can no longer fully perform its shock-absorbing function. In grade 2 pathology, bone structures change compensatoryly. To accommodate increasing loads, the joint platform flattens. Multiple bone spike-like growths (osteophytes) begin to form. The joint space narrows, and subchondral osteosclerosis occurs - compaction of bone tissue directly under the lower surface of the cartilage.
Clinical diagnosis
To assess the condition of the patient’s body, the doctor prescribes general clinical urine and blood tests. If synovitis occurs in the body in a latent form (as evidenced by the detection of leukocytosis and an increased level of ESR), this indicates the development of inflammation in the joint tissue.
In some cases, serological and biochemical studies may be required. This will help differentiate systemic and infectious diseases. Intra-articular fluid and cartilage tissue can also be collected to carry out a morphological study. This makes it possible to detect degenerative-dystrophic disorders in the articular tissue of the knee.
Diagnostic methods of the disease
Many inflammatory pathologies of the knee joint can be disguised as signs of grade 2 gonarthrosis. Therefore, to confirm the initial diagnosis made on the basis of the patient’s complaints and medical history, a number of studies are required.
Examination by an orthopedist
During an external examination, the orthopedist notes coarsening of the contours of the bones, deformation of the joint, and curvature of the axis of the limb. Transverse movement of the knee pad is accompanied by a crunching sound. During palpation, the doctor detects areas that are painful when pressed at the level of the joint space, as well as slightly above and below it. Functional tests are performed to assess range of motion and muscle strength. Grade 2 gonarthrosis is often accompanied by synovitis. Inflammation of the synovial membrane is manifested by swelling and redness of the skin. The contours of the knee are smoothed out, a rounded seal is formed, when pressure is applied to it, the movement of fluid inside is felt (fluctuation).
Clinical researches
General clinical blood and urine tests are prescribed to patients to assess their health status. In case of latent synovitis, their results (leukocytosis, increased ESR level) make it possible to identify the inflammatory process in the joint. If necessary, serological and biochemical studies are carried out to exclude systemic and infectious pathologies. In some cases, samples of synovial fluid and cartilage tissue are taken for the purpose of morphological study and detection of degenerative changes in the knee joint.
X-ray studies
X-ray is the most informative in diagnosing gonarthrosis of grade 2 severity. The resulting images clearly visualize a narrowing of the joint space, the proliferation of multiple osteophytes, and deformation of the articular areas of the bone (cyst formation, signs of subchondral osteosclerosis). The results of radiography often make it possible to establish the causes of the development of pathology, for example, improperly fused ligaments and tendons.
Ultrasonography
The technique makes it possible to identify early signs of pathological changes in the soft tissue structures of the joint. Therefore, ultrasound for grade 2 gonarthrosis is indicated only for assessing the condition of the synovial membrane, joint capsule, ligamentous-tendon apparatus, and periarticular muscles.
Magnetic resonance imaging
MRI is used to study joint damage in more detail. During the diagnostic procedure, it is possible to dynamically assess the blood circulation in the knee. The monitor screen displays blood vessels, nerve trunks, muscle tissue, cartilage and bone structures, ligaments, and tendons.
X-ray examination
X-ray diagnostics is the most informative when diagnosing stage 2 knee arthrosis. On the resulting x-ray you can see:
- how the joint space has narrowed;
- see multiple bone growths (osteophytes);
- see deformation of the bone tissue of the joint in the form of the appearance of cystic formations or signs characteristic of subchondral osteosclerosis.
Thanks to X-ray examination, it is most often possible to determine the cause of the problem, for example, incorrect fusion of ligament and tendon tissue.
Differences from other degrees
Grade 2 gonarthrosis is an intermediate stage of pathology. At this stage, following all medical recommendations will help avoid surgical intervention. In contrast to stage 3 disease, the joint space has healed slightly, so the range of motion has not decreased significantly. But moderate pain occurs more and more often, which is not typical for gonarthrosis at the initial stage of development. It is pathology of the 2nd degree of severity that is usually diagnosed in patients - they are forced to see a doctor by the gradual deterioration of their physical and, as a consequence, psycho-emotional state.
Causes
Most often, the primary form of knee arthrosis is detected in older people, mostly women. The consequence of the disease is the natural wear and tear of the cartilage in the knee joint. In young and middle-aged people, the cause of the disease often lies in excess load on the joint.
The development of secondary gonarthrosis occurs as a concomitant disease with the following health problems:
- Bekhterev's disease, reactive, psoriatic, chronic sluggish arthritis of an infectious nature;
- systemic diseases - systemic lupus, scleroderma, rheumatoid arthritis;
- endocrine, metabolic pathologies - gout, diabetes mellitus, hyperthyroidism, hypothyroidism;
- injuries suffered in the past - fracture of a tubular bone, rupture of the meniscus, ligament or tendon tissue, intra-articular fracture;
- disorders in the knee joint of a congenital and acquired nature.
A predisposing factor to the formation of arthrosis of the knee joint is the presence of excess weight, which is often accompanied by varicose veins. The development of this condition is facilitated by a sedentary lifestyle, smoking, and a lack of essential vitamins and minerals in the body.
When to see a doctor?
It is important to consult a doctor if the first signs characteristic of knee arthrosis are detected:
- prolonged and intense pain that increases with movement;
- periodic crunching in the joint area;
- restrictions in physical activity;
- noticeable knee deformity;
- swelling
If these symptoms occur, it is imperative to visit an orthopedic traumatologist for an examination and to undergo appropriate diagnostic procedures and prescribe therapy. You can also contact a rheumatologist or surgeon with similar complaints.
If there are no doctors of this specialization in the nearest clinic, it is recommended to contact your local physician - he will be able to advise where specialized medical care of this type is provided.
Symptoms of pathology
The leading symptom of grade 2 gonarthrosis is arthralgia, or joint pain. It occurs not only during movement, but also at rest, and can appear at night. Bending and straightening the knee is accompanied by a crunching sound due to the gradual exposure of the surface of the bones. In the morning the knee swells and looks larger than a healthy joint. After waking up, the patient feels stiffness of movement, which disappears within 30-40 minutes. If a small part of the destroyed cartilage gets between two bone surfaces, the joint “jams.”
Proper nutrition for gonarthrosis of the knee joint 2 degrees
If articular pathology is detected, the patient will have to follow some rules regarding his own diet:
- Eat jelly, jelly, jellied fish and other dishes containing gelatin.
- Eliminate regular table salt from your diet. As a replacement, you should use sea or iodized salt when cooking.
- Be sure to diversify your menu with fresh or boiled vegetables, fresh herbs, eggs, legumes, cereals, and bran.
- It is healthy to eat low-fat dairy products, marine fish, boiled beef in small quantities, chicken and rabbit.
- It is recommended to diversify your diet with herbal infusions, still mineral water, green tea, vegetable and fruit juices.
- Refractory fats of animal origin will have to be replaced with vegetable oils.
You will have to give up foods that contribute to the deterioration of the condition of joint tissue and the body as a whole:
- too salty and spicy dishes;
- smoked meats
- sweet sparkling water;
- fatty meat and fish products;
- lard, canned food, semi-finished products;
- buns;
- instant food products;
- mixtures containing preservatives and dyes.
During the day, it is necessary to drink clean water in an amount of about 2 liters, since a lack of fluid can negatively affect the condition of cartilage.
Restoring cartilage tissue requires an integrated approach to treatment. One of the components of therapy is a properly formulated diet. It is also important to reduce weight to a certain level in accordance with the patient’s age and height. Due to excessive stress on the affected joint tissue, healing is slowed down.
Lifestyle, useful tips
If, when visiting a doctor, you are diagnosed with stage 2 gonarthrosis, you will have to follow these recommendations:
- Maintain a positive mood. Although knee arthrosis cannot be cured, you should not despair. The degenerative-dystrophic process in the joint can be slowed down by using intra-articular injections (liquid endoprosthesis) with continued active lifestyle.
- Move as much as possible, starting the day with light physical activity on your legs, which can be done right in bed. Throughout the day you need to regularly load your joints. If you lead a sedentary lifestyle, you need to get up and do a little warm-up. Prolonged stay in a stationary position is harmful to joint tissue.
- Drink plenty of water. To maintain joints and metabolism in normal condition, the daily intake of clean water (in addition to tea, juices, coffee, soup) is 1 liter.
- Control body weight. This is necessary to reduce the load on the affected joint. To this end, you need to switch to healthy food, excluding from the menu chips and sweets, semi-finished products, factory-made chicken, sausage products and store-bought pates, yoghurts. These products can be replaced with vegetables, beans, rose hips, sauerkraut, cottage cheese, and dried fruit compote.
- Take chondroprotective drugs. Experts recommend regular treatment with chondroprotectors, and it is better to give preference to injectable agents.
- Take calcium-containing medications. A course of vitamin D is also sometimes recommended. To select the correct remedy, you should consult your doctor.
- Do not put too much stress on your knees when playing sports, as this causes the cartilage to wear out faster. This leads to the progression of the pathology. You need to properly combine activity and rest.
- Workout. For gonarthrosis, it is better to choose swimming, skiing or cycling, since these sports are low-traumatic. Swimming helps to activate blood circulation, pump up the periarticular muscles, and restore tone.
What complications can there be?
If a patient with grade 2 gonarthrosis does not seek medical help or does not follow medical recommendations, then he may soon be diagnosed with grade 3 pathology. At this stage, fusion of the joint space occurs, which leads to immobilization of the knee (ankylosis). A person loses the ability to take care of himself in everyday life and perform professional duties. The situation is aggravated by frequent hemorrhages in the joint, external subluxations of the patella, and the development of secondary reactive synovitis.
Gymnastics
A set of gymnastic exercises is selected by the attending physician in each specific case. During exercise, movements should be smooth and slow, no need to jump or squat. The optimal time to do exercises is in the morning. Each exercise should be done 10 times, 20 minutes should be allocated for gymnastics for training in a sitting and lying position.
The purpose of gymnastic exercises for gonarthrosis is to prevent the destruction of cartilage tissue, slow down the process of decreased mobility, activate blood circulation and relax muscle spasms.
Gymnastics Evdokimenko
The gymnastic complex of Dr. Pavel Evdokimenko was designed to be performed by patients during remission. When the pathology begins to worsen, performing these exercises is prohibited.
Dr. Evdokimenko has developed many different exercises, but one session will require a maximum of 10 of them. You need to train every day for half an hour.
Let's consider several exercises from the Evdokimenko gymnastic complex:
- Lie on your back, raise your lower limb 10 cm from the floor surface and fix it in this position for a couple of minutes.
- We sit on a chair, keep our back straight, straighten and lift first one and then the other leg in turn. We hold them in this position for 40-50 minutes.
- We stand near the chair, turn to face it and lean on the back. We rise on our toes and stay in this position for 3-5 seconds.
Gymnastics Popova
Gymnastic exercises were developed by the famous chiropractor and traumatologist Peter Popov. The training is perfect for patients suffering from left- or right-sided arthrosis of the knee joints, as well as bilateral gonarthrosis.
Let's look at some exercises from Popov's gymnastic complex:
- We sit on a chair and imitate walking, raising and lowering our heels.
- We lie down on the floor and turn to our side. Raise your leg up and lower it. Then we turn over to the other side and repeat the exercise with the other leg.
- We stand near the chair. Leaning against the back, we move one leg back a little and rotate the foot. Then we change the leg and perform the exercise with the second leg.
Before you begin performing such a gymnastic complex, you need to warm up the damaged joints by rubbing them with your palms. Any movements when performing such exercises should be performed measuredly.