A person’s daily life is unthinkable without physical activity, and therefore diseases that lead to a decrease in it are perceived as especially painful at any age. Osteoarthritis of the knee joint, also called gonarthrosis, occupies a special place among such diseases. The knee joint is located lower than most others, and therefore experiences the greatest load. It can occur not only when walking, but also when sitting in an uncomfortable position.
Over 75% of elderly people complain of symptoms associated with gonarthrosis. In advanced cases, even moving around the apartment becomes difficult—to get to the kitchen, the patient needs crutches or the help of loved ones. Osteoarthritis of the knee joints is one of the 10 main causes of disability in Russia. However, the disease can be prevented at a young age - in the early stages its development can be significantly slowed down, the main thing is to learn in time how to treat osteoarthritis of the knee joint.
Osteoarthritis of the knee joint. Causes
Osteoarthritis of the knee joint is a chronic disease in which degenerative-dystrophic changes in cartilage lead to complete destruction of the intra-articular lining. Clinical symptoms are pain, limited joint mobility.
More often, gonarthrosis is diagnosed in women 45+, professional athletes, overweight people engaged in heavy, monotonous physical labor.
It is impossible to name a single reason leading to the development of the disease. A number of unfavorable factors weaken cartilage. The onset of the disease is a fatal coincidence of circumstances.
Contribute to the occurrence of the disease:
- knee injuries (fractures, dislocations, meniscal injuries), surgical interventions on joints;
- aging (with age, cartilage loses its elasticity and cracks easily);
- systemic autoimmune diseases (rheumatism, rheumatoid arthritis, lupus erythematosus, etc.);
- endocrine pathologies (diabetes mellitus, hypothyroidism), menopause;
- genetic factors (vulnerable cartilage tissue, insufficiency of synovial fluid);
- excess weight (excessive load on joints);
- hypothermia and dehydration;
- overload of the knee joints during heavy work and sports;
- pathology of the hip joints.
Low physical activity also contributes to the development of arthrosis. With a sedentary lifestyle, the blood supply to the lower extremities decreases, metabolic processes slow down, muscles, ligaments, tendons atrophy, and cartilaginous structures degenerate.
Endoprosthetics
Endoprosthetics
- computer navigation systems are used that perfectly calculate all angles, distances and biomechanical axes when installing an endoprosthesis;
- new, increasingly high-quality artificial joints are appearing, almost completely areactogenic (not rejected by the body), very functional (providing a high range of motion), capable of serving for decades;
- Minimally invasive techniques for installing artificial joints are used with minimal damage to soft tissue, which shortens the rehabilitation period and reduces the risk of complications.
Already on the first day after endoprosthetics, a person is recommended to put weight on the operated leg. Rehabilitation lasts several months. After six months or a little more, the person is allowed to bear full weight on the operated leg.
Symptoms of osteoarthritis of the knee joint
The course of the disease is variable and depends on the age and physical condition of the patient, the cause of the pathology, and concomitant diseases. As a rule, pain in the knees during exercise, swelling, burning in the affected joint, numbness after prolonged immobility, dry crunching, clicking when moving are a concern.
The diagnosis of the disease is made by an orthopedic doctor after examination, questioning and additional examinations.
Osteoarthritis of the knee joint 1st degree
The disease is often asymptomatic. Sometimes patients experience slight discomfort, tension, and warmth in the knee joint.
A typical clinical picture of first degree gonarthrosis includes:
- pain during movement or at rest after significant loads, at the moment of maximum flexion and extension;
- burning, swelling and hyperemia of the knee after exercise (symptoms of inflammation);
- X-ray examination reveals single osteophytes and narrowing of the joint space.
Important!
Clinical symptoms typical of the first stage of the disease may be accompanied by significant destruction of cartilage. Timely diagnosis is important, since conservative treatment is more effective at the initial stage of the disease.
Osteoarthritis of the knee joint grade 2
The pain becomes more intense and prolonged, the functionality of the joint is limited (the amplitude of voluntary movements decreases). The knee joint begins to deform due to uneven wear of the cartilage (“flattened”), and pathological bending of the lower limb is possible. Typical signs of grade 2 osteoarthritis:
- constant pain during exercise, more pronounced in the morning and evening;
- persistent discomfort in the joint even after a long rest;
- decreased range of motion;
- increase in joint volume, atrophy of periarticular soft tissues;
- crunching noise during sudden movements, squats, and sometimes when walking.
X-ray examination reveals osteophytes, narrowing of the joint space is possible up to 30-40%. As a rule, medical help is sought precisely at this stage, when the quality of life is significantly reduced.
Osteoarthritis of the knee joint 3rd degree = deforming osteoarthritis of the knee joint
At the final stage, the disease disables the patient, since the cartilage tissue is almost completely destroyed, the joint space is narrowed to the maximum, and sometimes absent. Multiple osteophytes and deformation of articular segments of bones are determined. It is possible to block the joint due to a fragment of osteophyte getting into the joint space. The leg is not functional and constantly bothers me. Movement is often only possible with the help of a cane, crutches, or walker.
The following symptoms are typical:
- constant pain in the joint;
- severe deformation of the joint;
- immobility of the knee joint;
- lameness when walking, there may be shortening of the limb;
- swelling of the joint due to excessive accumulation of intra-articular fluid;
- numbness of the leg, decreased sensitivity;
- significant atrophy of the musculo-ligamentous apparatus of the joint.
Osteoarthritis affects joint bone tissue, increasing the risk of fractures. At this stage, only surgical treatment is effective. Conservative methods help reduce pain, slightly increase range of motion, and temporarily improve quality of life.
Frequently asked questions about the disease
Is it possible to stop deforming arthrosis?
Not only is it possible, but it is also necessary. Only a doctor can do this.
How quickly does arthrosis deformans progress?
It all depends on genetics, lifestyle and compliance with doctor’s orders.
Which doctor treats you?
Depending on the cause of development, this can be done by an orthopedic traumatologist or rheumatologist.
What prognosis do doctors usually give?
It is quite possible to stop the progression of the disease and improve the quality of life at any stage.
Can children develop the disease?
Yes, against the background of congenital malformations of the joints, as well as after illnesses and injuries.
Arthrosis deformans is a long-term, constantly progressive disease. If left untreated, excruciating pain and disability are guaranteed. Only a doctor can help, but it is very important to choose a clinic with experienced specialists. The doctors of the Moscow Medical Center have such experience, they will definitely help you!
Literature:
- Alekseeva L.I. Modern approaches to the treatment of osteoarthritis // Breast cancer. 2003. T. 11. No. 4. pp. 201–205.
- Reginster JY, Deroisy R, Rovati LC et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomized, placebo-controlled clinical trial// Lancet. 2001; V. 357: 251–256.
- Hajjal HEL, Marcelis A., Devogelaer JP, Manicourt DH Celecoxib has a positive effect on the overall metabolism of hyaluronan and proteoglycans in human osteoarthritic cartilage // J. Rheum. 2003; 30:2444–2451.
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 10/29/2021 Date of update: 11/04/2021
Reader rating
Rating: 5 / 5 (1)
Signs of osteoarthritis of the knee joint
The main clinical symptoms of the disease: knee pain, limited mobility, joint deformity, aseptic inflammation of the synovium (synovitis).
Knee pain
Pain in the joint can vary from severe, limiting joint mobility, to barely noticeable with certain movements. In the initial stages of OAC, the pain is insignificant and occurs with prolonged sitting in an uncomfortable position, long walking, or lifting heavy objects. They go away quickly after rest and get worse in cold and damp weather.
The cause of severe pain in the knee is reactive inflammation of the joint (synovitis) or periarticular soft tissues (muscles, tendons, bursae). When periarticular soft tissues are involved in the inflammatory process, the pain intensifies with certain movements, and “starting” pain is characteristic (pain and stiffness after a period of rest).
Limitation of joint mobility
Due to the destruction of cartilage, the proliferation of osteophytes, and a deficiency of synovial fluid, the biomechanics of the joint is disrupted, which leads to a limited range of movements up to complete immobility in the last stage.
Knee deformity
Due to the uneven destruction of cartilage and subchondral bone tissue, the joint loses its usual shape (deforms). The muscles, tendons, and ligaments that form the joint atrophy.
Synovitis
Synovitis is a reactive inflammation of the inner lining of the joint. Aseptic (microbial-free) inflammation inside the joint occurs due to irritation and damage to the synovial membrane with pieces of destroyed cartilage. The inflammatory pain is intense, intensifies with movement, the knee increases in volume. The process subsides on its own, but can resume under unfavorable conditions.
Pathogenesis of arthrosis of the knee joints
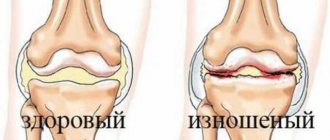
Morphologically, arthrosis is wear and tear of the cartilage lining of the joint, leading to disruption of the normal anatomical structure of the articular surfaces. The joint is formed by the articular surfaces of the tibia and femur, covered with cartilage tissue. During movements, cartilage acts as a shock absorber. Cartilage consists of connective tissue fibers loosely located in a jelly-like substance (matrix). Due to the matrix, cartilage is nourished and regenerated.
Cartilage tissue is like a sponge: at rest it absorbs fluid, and when loaded, squeezes it into the joint cavity, allowing the bones to glide. Under load, some of the fibers are worn out and destroyed. Normally, they are replaced by newly synthesized ones. Osteoarthritis occurs when there is an imbalance between the synthesis of cartilage and its destruction.
Damaged, less complete cartilage structure absorbs less fluid, drier and more brittle cartilage easily splits under stress. The structure of the underlying bone changes - osteophytes grow along the edges of the joint, compensating for the loss of cartilage by the growth of articular surfaces.
Not only the cartilaginous covering of the joint suffers; meniscal tears, cruciate ligament injuries are periodically diagnosed with DOA, and sometimes loose intra-articular bodies are detected. Due to partial or complete destruction of the cartilage and subchondral plate, the contact surfaces are displaced, causing the joint to become deformed.
Deforming osteoarthritis of the knee joint is arthrosis of the last stage.
Primary arthrosis of the knee joint
Primary ACS is considered if the immediate causes of the disease have not been identified (there were no injuries, no concomitant diseases, no professional history).
Secondary arthrosis of the knee joint
Secondary AKS is degenerative-dystrophic changes in the knee joint due to metabolic diseases (diabetes mellitus, gout), rheumatoid diseases (rheumatoid arthritis), vascular pathology (vasculitis, atherosclerosis) or in the presence of a professional history (sports, heavy physical labor) .
Endoprosthetics
Advanced arthrosis sooner or later requires joint replacement. This is the main treatment method for such patients. Millions of such operations are performed annually around the world. They are becoming more and more effective and safe.
The essence of the operation is that the person’s own joint is removed. An artificial endoprosthesis is installed in its place. It has sufficient functionality for a person to lead a physically active lifestyle. Even operations carried out over decades were mostly successful. Today their effectiveness is even higher because:
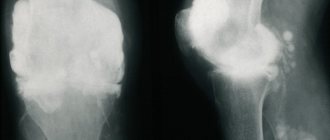
Diagnostics
To verify the diagnosis, special examination methods are prescribed. The most informative are: X-ray, magnetic resonance imaging and arthroscopy. X-rays reveal narrowing of the joint space and deformation of the articular surfaces. The degree of damage to cartilage, menisci, and ligaments can be assessed using an MRI examination.
Diagnostic arthroscopy is an examination of articular cartilage using endoscopic equipment. Softening and degeneration of the articular lining (chondromalacia) of varying severity are detected.
1st degree. Superficial damage to articular cartilage. The cover is uneven, degeneratively changed.
2nd degree. Deep destruction - fiber disintegration, cracking.
3rd degree. Profound changes, pronounced thinning of cartilage.
4th degree. Through defects of cartilage with exposure of underlying bones.
Osteochondral mosaic plastic surgery
Osteochondral mosaic plastic surgery
- the presence of a limited defect of articular cartilage no more than 4 square centimeters;
- good quality of the cartilage surrounding the articular defect (pathological changes no more than grade II according to Outerbridge);
- the defect is located in the loaded area of the femoral condyle;
- There is donor material in sufficient quality and quantity.
For extensive defects of the cartilage surface, surgery is not performed. It is also not performed if it is impossible to obtain sufficient quantities of high-quality cartilage tissue from donor areas of the body.
Abrasive chondroplasty
This is a palliative operation. It reduces pain but does not prevent further wear and tear of the cartilage. During surgery, the hyaline cartilage is “polished.” Damaged fragments are removed. The thickness of the removed layer is 1-3 mm. After the procedure, a blood clot forms and cartilage-like tissue forms to cover the defect. The technique gives good early but poor delayed results. The operation does not have a drastic effect on the outcome of arthrosis.
Classification of ACS
According to the Kosinski classification of ACS, three stages of the disease are distinguished according to radiological and clinical manifestations. They focus on the degree of narrowing and unevenness of the joint space, deformation of the articular surfaces, changes in the subchondral bone (osteosclerosis).
First stage of gonarthrosis
The changes are almost invisible. The joint space is normal or slightly narrowed, with isolated tiny osteophytes at the edge of the articular surfaces.
Clinically - mild short-term pain after significant fatigue, minimal impairment of knee function. Most do not perceive these symptoms as a pathology and do not seek medical help.
Second stage of gonarthrosis
The joint space is unevenly narrowed by 2-3 times. Maximum narrowing in places of maximum load (usually the inside of the joint). Along the edges of the articular surfaces there are large osteophytes, sclerosis of the endplate, and subchonar bone cysts. Moderate deformation of the bone epiphyses, disruption of the congruence of the articular surfaces.
Clinically - dysfunction of the knee in the form of limited movements, crunching, limping. Often there is slight local swelling and atrophy of the periarticular soft tissues.
Third stage of gonarthrosis
The intraarticular gap is barely noticeable or has disappeared. Many sharp massive osteophytes completely surround the articular surfaces. Gross deformation of the articulating surfaces (expansion and flattening), osteosclerosis of the epiphyses of the bones forming the joint, the presence of cysts. The joint is deviated from the vertical axis.
Clinically - visual deformation of the knee (thickening), forced position, immobility. Atrophy of all muscles of the lower limb, especially the quadriceps. Lameness, movement with the help of crutches, canes, walkers, constant excruciating pain. Patient's disability.
Treatment of arthrosis of the knee joint
Treatment of arthrosis of the knee joint is complex, including drug therapy, physiotherapy, surgical interventions, therapeutic exercises, and diet therapy. The range of therapeutic measures depends on the degree of cartilage destruction and clinical manifestations.
Conservative treatment gives a positive result in the first, partly in the second stage of the disease, while most of the cartilage is not yet destroyed.
Drug treatment
Non-steroidal anti-inflammatory drugs (diclofenac, ketoprofen, indomethacin, meloxicam, etc.) are used to relieve pain and inflammation. It is not recommended to take them for a long time, as they negatively affect the synthesis of proteoglycans, which causes dehydration and accelerated cartilage destruction. In addition, they have unwanted side effects from the gastrointestinal tract.
Chondroprotectors (glucosamine and chondroitin sulfate) nourish cartilage tissue, promote regeneration, improve the production of intra-articular fluid, and normalize lubricating properties. Chondroprotectors are ineffective in the third stage of gonarthrosis, when the cartilage is practically destroyed. To obtain a real treatment result, 2-4 courses of treatment are needed (lasting up to one and a half years).
Glucocorticosteroids (diprospan, hydrocortisone, celeston) quickly and effectively relieve pain and inflammation during synovitis, but arthrosis itself is not treated. The first injection of GCS relieves symptoms more effectively than all subsequent ones. They have many side effects and, with frequent use, negatively affect cartilage tissue. Moreover, glucocorticoids are dangerous for diabetes mellitus, arterial hypertension, renal failure, and peptic ulcer disease.
Hyaluronic acid preparations are a modern and safe way to treat arthrosis. Act in the joint as a natural synovial fluid. Sodium hyaluronate covers damaged cartilage with a protective film, preventing further destruction and improves gliding. Penetrates deep into the cartilaginous lining, improving firmness and elasticity, restoring shock-absorbing properties. They start the process of producing their own hyaluronic acid. As a result, the biomechanics of the joint is normalized, pain is relieved, and mobility is restored.
Important!
HA drugs are destroyed in the inflamed joint. Therefore, you first need to stop the symptoms of synovitis with the help of GCS and NSAIDs.
HA preparations:
HYAL-SIN - 1% high molecular weight hyaluronic acid. The course of treatment includes three injections with an interval of 7-10 days.
HYAL-SIN PROLONG - 2% high molecular weight hyaluronic acid. The high concentration of hyaluronic acid makes it possible to reduce the course of treatment to two injections, while simultaneously enhancing the intra-articular effect of the drug and prolonging the effect.
GYAL-SYN PROLONG PLUS -2% long-acting high molecular weight HA (12-24 months) for single use. Intermolecular cross-linking of the HA chains of this drug is carried out for a longer effect and resistance to destruction. One injection per course of treatment. Applicable only to the knee joint.
The most effective is an integrated approach: when all methods of conservative therapy are used.
Surgery
For advanced forms of KLA, the method of choice is knee replacement. This is the replacement of the knee joint with a functional endoprosthesis. Implants made of high-tech alloys (titanium, cobol-chromium, etc.) are strong, rigid, elastic, and biocompatible with human tissue.
Endoscopic arthroscopy with minimally invasive manipulations is performed if the course of the disease is complicated by ruptures of the ligaments, meniscus, or the entry of a bone fragment into the joint capsule.
Physiotherapy
Complex treatment of stages 1-2 of OAC includes shock wave therapy, ultrasound, manual techniques, iontophoresis, mechanical traction of the joint, laser therapy, thermal treatment, cryotherapy (local cooling). A good effect is obtained by combining manual therapy with traction.
Diet therapy
Age-related osteoarthritis is associated with the loss of calcium salts, which provokes microcracks in bones and fragility of osteophytes. Patients with OAC are advised to follow a non-strict diet, which includes:
- consumption of lean meat, fish, seafood;
- introduction of high-protein ingredients (nuts, legumes, wheat germ) into the diet;
- dishes that include plant and animal collagen (jelly, aspic, jellied meat);
- dairy products;
- ban on fatty, salty, spicy foods.
People who are overweight are prescribed a more strict diet to lose weight.
Physiotherapy
Therapeutic gymnastics strengthens muscles and activates blood circulation in the joint. Use exercises without maximum flexion and extension. Instead of the usual dynamic exercises, static ones are used. For example, lying on your back, raise your outstretched leg and keep it suspended for some time.
Important!
To strengthen muscles and ligaments, do static or slow dynamic exercises. If the exercise causes sharp pain, then it is contraindicated or performed incorrectly.
Are injections effective: injection injections are different
Intra-joint injections today aim not only to reduce inflammation and alleviate the patient’s condition. Modern drugs are many times more effective than chondroprotectors in restoring articular cartilage by renewing synovial fluid. Today intra-articular injections of the following drugs are practiced:
- Glucocorticoids.
They allow you to quickly eliminate pain and relieve inflammation, but do not improve the condition of the cartilage. They can be used only in the acute period, with synovitis, when other methods are contraindicated. The drugs are hormones, so their frequent administration stops the regeneration of cartilage, and with excess weight, hypertension, peptic ulcers and other diseases, side effects often occur.
- Hyaluronic acid.
Such preparations are also called “liquid prostheses”. Once inside the joint, they act as natural synovial fluid, lubricate the surfaces, and stimulate the restoration of cartilage. Products based on hyaluronic acid can cause allergies. Their validity period is only a few months, since immune cells in the human body contribute to the rapid breakdown and elimination of the drug.
- Synthetic synovial fluid substitutes, such as Noltrex
Noltrex is an artificial endoprosthesis that also replaces synovial fluid and restores its normal viscosity. Unlike natural-based drugs, it contains no components that would be broken down by phagocytes. That is why the medicine remains at the injection site for a long time and provides a long-lasting effect - up to one and a half to two years.
Synthetic Noltrex is absolutely safe and hypoallergenic
Forecast. Prevention
Osteoarthritis of the knee joint is difficult to treat and is one of the ten main causes of disability in the Russian Federation and Belarus. However, in the early stages, the progression of the disease can be significantly slowed down. If there are risk factors for the purpose of prevention, it is recommended to:
- balanced loads on joints (optimal training and work regimen);
- swimming;
- massage of thigh and calf muscles;
- maintain optimal weight;
- rejection of bad habits;
- regular physical therapy exercises;
- wear comfortable shoes, do not get too cold, do not overwork;
- diet therapy;
- treatment of concomitant diseases.
Long-acting hyaluronic acid preparations GIAL-SIN, GIAL-SIN PROLONG, GIAL-SIN PROLONG PLUS will improve trophism and slow down the degeneration of the cartilage lining of the knee. Course treatment is the key to achieving a positive effect. The duration of therapeutic and preventive action is 12-24 months.
Approach to treating the disease in our clinic
Specialists at the Paramita clinic in Moscow not only use all modern methods of diagnosing and treating osteoarthritis, but also actively use traditional oriental methods. Such as reflexology (acupuncture, moxibustion, acupressure), herbal medicine, etc.
Each patient is unique to us. This approach allows you to quickly eliminate pain and significantly speed up the process of treatment and rehabilitation of patients with deforming arthrosis. With regular maintenance treatment, our patients forget about their problems and lead a normal lifestyle.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis