Arthrosis of the knee joint is a degenerative-dystrophic pathology that leads to deformation and destruction of articular cartilage. Gradually the limb loses mobility. According to statistics, almost every third person on the planet suffers from arthrosis, and this number is not decreasing. Elderly people, especially those who are overweight, are at risk. After 65 years, arthrosis is diagnosed in 70-85% of cases of treatment for knee pain.
A rheumatologist helps maintain a patient’s quality of life with joint pathology.
Features of the development of osteoarthritis of the knee joint
Osteoarthritis of the knee joint
is a common pathology that belongs to the category of the most common diseases that have an extremely negative impact on a person’s quality of life.
Degenerative-dystrophic processes most clearly manifest themselves in the form of physical dysfunction of the legs, accompanied by severe pain. Depending on how much the pathological process progresses, further forecasts for the course of the disease are made.
One of the disappointing forecasts is paralysis of the lower limbs. The seriousness of the consequences of pathological processes necessitates seeking qualified medical help.
Treatment 2 degrees
With gonarthrosis of moderate severity, the quality of life already becomes significantly spoiled. A sore knee worries more, the painful syndrome manifests itself more often and more intensely than it was at the beginning of the disease. The pain is especially pronounced immediately after waking up in the morning, while going up and down the stairs. There is often a feeling of unpleasant numbness that appears after prolonged walking or standing in one position for a long time. Flexion in the knee area is reduced, the patient is not able to bend the leg, as required by physiology. A person begins to spare his limb, trying almost not to step on it, which is why gradual muscle atrophy occurs.
It’s still tolerable, but often the knee makes itself felt.
It is strictly prohibited to undergo treatment at home without seeking medical help from a professional orthopedist! If the deformity becomes more complex, it will lead to immobilization and blocking of the joint. That is why adequate diagnosis and equally competent treatment in accordance with the nature of the disorders are extremely important, and not classes according to Bubnovsky. According to the well-known Bubnovsky method, you cannot train everyone, if only because it does not take into account the individuality factor of each individual medical problem. In addition, it can be useful only in the initial period, while physical rehabilitation should be carried out in conjunction with the main treatment program.
But the pool is always recommended to everyone; there are practically no contraindications to it, with the exception of open or fresh wounds.
We emphasize that treatment necessarily involves a qualified, comprehensive approach.
- If the doctor does not see an urgent need for surgery, the priority is to reduce the load on the problem area. If you are overweight, in order to ensure good relief for the joint affected by arthrosis, it is imperative to adjust your body weight by following the diet that your doctor recommends.
- All patients are prescribed the use of special orthopedic devices when moving. This, depending on the existing problem, may include knee braces, compression garments, elastic bandages, a cane, crutches, or a walker.
- Additionally, the orthopedic traumatologist will prescribe a unique set of exercises that will help strengthen and increase the endurance of the muscles of the affected limb.
- Also, arthrosis in moderate to moderate manifestations involves the use of medications that include substances present in the cartilaginous tissues of the knee. These include formulations based on chondroitin sulfate, injections of hyaluronic acid, and preparations with glucosamine. They cannot restore cartilage, but saturate it with nutritional components, so that remission of the disease can be achieved.
- Physiotherapy procedures are also recommended, but they are used only after all signs of inflammation have disappeared. Physical sessions, for example, laser, magnet or ultrasound, should take place within the medical facility. Thanks to physiotherapy, nutrition and metabolism in bone, muscle, and cartilage tissues improves. If you bought a Vitafon vibroacoustic device for home use, first ask a specialist about the possibility of using it for your diagnosis and the operating features of the device.
We have reviewed the basic principles on which the official treatment of arthrosis is based, meeting the standards of orthopedics. Since many people with stage 2 osteoarthritis. are very interested in alternative methods, looking for their salvation in them, we offer to get acquainted with the most popular of them. And let’s find out whether they are as unique as they are presented to us on the Internet.
Stem cells for knee treatment
We will talk about autotransplantation of mesinchemal stem cells to a patient with knee gonarthrosis, taken from the crest of the pelvic or femur. Cell therapy, according to interested sources, will achieve almost self-renewal of the entire joint by activating regenerative self-healing processes in the damaged segment. Thanks to this technology, it is theoretically possible to achieve improvement in the constituent units of the osteochondral organ. However, in practice, there is not yet a single “live” radiographic evidence that would confirm that after the introduction of stem cells into the affected area, the joint became healthy.
It is possible that this technology is the future, but as a rule, when introducing new methods, the percentage of failures of varying degrees is never announced, so at this stage it is better not to experiment.
The positive effect of stem cells on joints and bones has not been proven and is highly doubtful, since this technique has not yet been recognized in orthopedics. Scientists are just studying and experimenting with it. Moreover, there is information regarding the unsafe effect of stem cells on the human body, which, according to highly competent specialists, can provoke cancer. What about those people who paid for the procedure and were satisfied with the result? Here we can only say one thing: many patients will believe in eternal life for that kind of money, but the placebo effect does not last long, do not forget about this too.
Method according to Neumyvakin
Treatment of the knee joint according to the method of Neumyvakin, a professor of space medicine, involves the use of ordinary hydrogen peroxide orally (orally), by injection or locally (in the form of compresses, lotions on the knee). Traditional orthopedic doctors have an extremely, extremely negative attitude towards this method. But Neumyvakin assures that in order to restore your joint, you need to prevent oxygen starvation of cells and tissues, and everything will return to normal. For oral administration, peroxide is diluted in water and drunk according to a specific regimen.
Professor Neumyvakin.
Attention! Internal intake of peroxide leads to damage to the gastrointestinal tract, and is also often accompanied by all sorts of severe adverse reactions, ranging from gastritis to urticaria, diarrhea, cough, rhinitis and lethargy. It is difficult to predict how your body will react to this remedy, so it is better not to take risks. And remember that you cannot take any medications in parallel with oxygen therapy! As for any lotions and the like, applying a pharmaceutical solution to the skin, in principle, does not threaten life, but it will have no more than a mild analgesic effect.
Mud treatment
Therapeutic mud springs containing unique components (magnesium, chromium, iodine, bromine, calcium nitrate, etc.) help reduce painful symptoms, increase blood flow to diseased areas, and stimulate metabolism. They are of greatest value for people with a mild stage of the disease or patients who have already undergone surgery on the leg. It is also permissible to carry out mud therapy at level 2 if the doctor believes that a natural remedy in combination with the main treatment program will reduce the aggression of pathological phenomena (stop progression) and improve the overall clinical picture. Mud therapy is practiced in special health resort-type medical institutions. Natural healing muds based on peloids are used in the form of applications and in combination with the galvanization method (electrophoresis).
Uses of gelatin
Natural gelatin is a safe product that helps maintain joint structures in good condition. The jelly-like substrate, diluted in water, is recommended to be consumed internally. According to reviews of some doctors, gelatin will have a faster and more productive effect on bone, cartilage and muscle-ligamentous elements. Experts emphasize that this method does not have medicinal properties, it only helps prevent arthrosis. Consequently, if the pathogenesis has already taken place, gelatin treatment in the absence of pathology or at the earliest stages can be considered solely as a measure to prevent the appearance or progression of degenerative changes. When the disease is moderate and severe, this approach will not work for preventive purposes.
Gelatin is a good dietary supplement for keeping joints healthy, but not for treating them. The process of destruction of cartilage tissue is not reversible.
Ayurveda for joints
Modern alternative medicine is known for many extraordinary trends, including Ayurveda treatment of various parts of the musculoskeletal system. According to this unofficial theory, joint damage is associated with excess toxins accumulated in the body due to energetic disharmony. The damaging mechanism of disturbed energy balance (Vata) is primarily the weakening of Agni, or digestive fire, which leads to the accumulation of undigested food residues (Ama) in the intestines. They secrete toxins, which the blood transports to the joint, where harmful substances settle and inhibit metabolic processes.
Don't be fooled!
Let's be honest, this is not medicine, but pure philosophy, although it is possible that the emergence of a pathogenic environment in the knee joint in some patients developed according to this mechanism. According to Ayurveda, osteoarthritis is classified into several types, and each type has its own treatment system, each of which is based on diet, herbal medicine, taking Ayurvedic tablets and powders, yoga and breathing exercises, unconventional massage, auto-healing training, etc. Of course, all this sounds tempting, but if arthrosis cannot be reversed even through scientific high technologies, how can one believe that herbal powders, thought treatment and other Ayurvedic tactics will cure irreversible deformities?!
Salt compresses
We offer for consideration another common method - treatment of the knee joint with salt compresses. Salt (table and sea) is used to prepare a saturated saline solution used to impregnate compresses that are applied to the sore spot for several hours. Such therapy should not be considered as an independent remedy, much less as a panacea for gonarthrosis. Salt can temporarily soothe pain, relieve swelling of the soft tissues covering the bone structure, without harm to biological structures. But it will not cure the disease and will not put the patient back on his feet! Its effect is purely symptomatic. The solution is prepared at the rate of taking 100 g of salt per 1 liter of room temperature water.
For certain types of knee diseases, hot compresses can only do harm. Be careful.
Worth checking out! Sometimes salt is used in dry, heated form, which is placed in a bag, and local heating of the knee is performed. Sometimes as wet but hot dressings. Hot procedures are dangerous in case of purulent-inflammatory processes in the joint cavity; they will only aggravate the clinical picture to the utmost. Therefore, do not use such recipes without being sure that the lesion is not accompanied by a similar process.
What causes lead to knee arthrosis?
To identify the causes of arthrosis of the knee joint, it was necessary to conduct a large number of studies. Many years of examinations of patients and a thorough study of the clinical picture of the pathology allowed specialists to come to the conclusion that the influence of a number of negative factors is the root cause of the destruction of joint tissue, causing severe pain and inflammation.
Among the main reasons leading to degenerative-dystrophic processes, it is worth highlighting:
- previous injuries - a bruise, dislocation or fracture of the knee automatically classifies a person as a risk group and can cause the development of the disease. Damage to the joint presupposes its fixation, and long-term immobility is a direct path to the formation of arthrosis;
- strong physical activity - intense stress on the knees (especially in older people) leads to microtraumas, which also leads to the development of negative pathological processes;
- insufficiently strong ligamentous apparatus - abnormal joint mobility also negatively affects their condition, which manifests itself mainly in old age;
- excess body weight - extra pounds can cause irreparable damage to the knee joints, because the likelihood of meniscus injuries in this case is incredibly high. If a lot of weight is accompanied by varicose veins, then there is a high probability of developing severe forms of arthrosis of the joints of the lower extremities;
- metabolic disorders - a failure in the exchange of nutrients and elements in the body provokes the development of various kinds of diseases, which is caused by insufficient supply of various tissues, in particular bone and cartilage;
- increased levels of stress - worries and worries negatively affect not only people’s mood, but also the level of physical well-being.
Causes of knee pain due to osteoarthritis
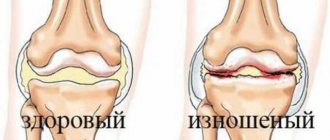
The knee joint is very strong, and daily supports the weight of the human body, and also endures enormous loads when carrying heavy loads and loads. It can be damaged by a strong blow, but even in the absence of a fracture or dislocation, there is a possibility of long-term pain that increases over time. This is caused by microdamage to the cartilage tissue, which acts as a protective shell for the joint. Over time, this small crack begins to enlarge and grow, causing stronger sensations of discomfort, hindering movement, and over time does not even allow the person to move, leaning on the sore leg.
Characteristic symptoms of arthrosis of the knee joint
The symptomatic manifestation of the disease allows timely tracking of the onset and development of pathological processes, which gives each patient the opportunity to recover.
Before determining who to turn to for help and how to treat arthrosis of the knee joint, it is important to become familiar with the symptoms of the disease.
Only a specialist competent in this matter can identify the presence and confirm the diagnosis by prescribing treatment for knee arthrosis. However, every patient should know the main symptoms of knee osteoarthritis, among which are usually identified:
- pain - discomfort that gradually develops into painful sensations does not appear immediately. Their slight manifestation in the knees can bother a person for many years, but at some point they may become stronger, and they will not stop in a calm state;
- crunch – “clicks” when flexing/extending a joint are an alarm bell, which manifests itself already in the second and third stages of the disease;
- synovitis is an inflammation of the joint membrane, in which fluid accumulates, which leads to local swelling;
- deformation is a characteristic feature that appears in the last stages of the disease, accompanied by pronounced inflammation and swelling.
Clinical picture at the middle stage
Pathological disorders of moderate severity are more intense than at an early onset. Painful sensations intensify and become more frequent; they can no longer go unnoticed. In addition to morning pain and discomfort after a long stay in a maximally immobilized state, pain syndrome naturally appears after walking and physical activity, and much more often begins to disturb for no apparent reason. When going up and down stairs, a person experiences difficulties, since the flexion/extension of the joint is already seriously limited.
Steps can be an insurmountable challenge.
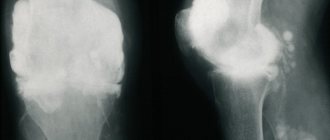
As for the results of the X-ray examination, they usually contain the following content:
- in direct and lateral projections, a significant narrowing of the joint space is clearly visible (2-3 times the required norm);
- a change in the density of articular cartilage is detected;
- there are large osteophytes at the ends of the articulating bones;
- there is pronounced subchondral osteosclerosis of the surfaces;
- the first deformations of the bones and the curvature of their axis are visualized.
Due to pathological transformations and acute pain, a person protects the problematic leg in every possible way, trying to transfer the main part of the load to the healthy limb. Due to the forced gentle regime, muscle structures weaken, lose their functional tone, decrease in volume, in other words, they gradually begin to atrophy. Muscle atrophy further complicates motor problems: along with inadequate range of motion during exercise, lameness appears. Due to the destruction of cartilage, non-physiological sounds are felt in the knee at the moment of movement - crunching, clicking. The contracture is moderately expressed.
Diagnosis of arthrosis of the knee joint
Diagnosis and treatment of arthrosis of the knee joint is carried out by an orthopedist or rheumatologist. If you wish to undergo a diagnostic examination, each patient can contact a therapist, who will give a referral to a specialist or independently take a voucher to one of them.
The main diagnostic tool of specialists is, of course, an X-ray machine. Thanks to the image taken, you can track not only the presence of pathology, but also the degree of its development.
It is important to note that x-rays can exclude the possibility of the presence of other diseases of the musculoskeletal system.
X-ray examination opens up the opportunity for a specialist to:
- track the narrowing of the joint space;
- detect compaction in joint tissues.
The combination of clinical symptoms and information obtained from the image provides high-quality diagnosis and diagnosis, with the determination of further treatment for osteoarthritis of the knee joint.
Methods for diagnosing gonarthrosis
In case of constant or recurring knee pain, you should consult a doctor - a surgeon or orthopedic traumatologist. At your initial consultation, your doctor will ask you to describe your symptoms, noting when they began and how they appear. You may have had knee injuries, be sure to tell your doctor about them. Your doctor will then perform a physical examination of your knee using various tests to evaluate the mobility and functionality of the joint.
Instrumental diagnostics
The final diagnosis is usually made on the basis of x-rays. However, subtle wear of cartilage is difficult to notice on x-rays. Therefore, in such situations, computed tomography (CT) or magnetic resonance imaging (MRI) is usually performed.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Degrees of osteoarthritis of the knee joint
Modern medicine divides knee arthrosis into several degrees, in accordance with the nature of the development of pathological processes.
To begin with, it is worth noting that according to observations, the disease can have a different nature:
- unilateral (right-sided/left-sided);
- bilateral.
In addition, the pathological process has three stages of development, each of which has its own clinical picture.
1st degree arthrosis of the knee joint
The initial stage of the development of pathology, the successful diagnosis of which is an incredible success not only for the patient, but also for the attending physician.
The peculiarity of the degree of development of arthrosis at this stage is the absence of clinical signs and clear symptoms. Identification of the disease can be carried out during medical examination or during the study of another disease.
Evidence of grade 1 arthrosis of the knee joint may be:
- local discomfort in the knee area during long walking;
- mild pain that disappears with rest.
It is important to note the fact that pain can be felt in one or both joints of the lower extremities.
It is interesting to note that left-sided gonarthrosis is often diagnosed in left-handed people, while right-sided gonarthrosis is typical for people involved in various sports.
2nd degree arthrosis of the knee joint
Symptoms of the second degree of development of pathology are accompanied by an expansion of signs, which are usually included:
- pronounced pain syndrome;
- stiffness and severe discomfort in the knee joint;
- atrophy of the muscles located near the knee joint, which is caused by tissue damage;
- increased pain;
- visually noticeable deformation of the joint;
- limitation of mobility.
Expanding the symptoms simplifies the diagnostic process. Changes characteristic of grade 2 arthrosis of the knee joint are easy to track during palpation. When undergoing a clinical examination, a specialist can easily detect an abnormal formation in the knee area.
3rd degree arthrosis of the knee joint
It is almost impossible not to notice the third degree pathology, because the patient faces constant pain. In addition, the progress of the disease reaches a critical point, which is manifested by severe deformation of the joint, in which the limb completely loses the ability to flex/extend.
The lack of proper treatment leads to complete destruction of the cartilage and, as a consequence, the development of ankylosis (fusion of articular bones).
The only solution for the final stage of development of the disease is an expensive surgical intervention, involving the removal of remnants of cartilage tissue or joint replacement.
Brief description of the disease
Cartilage tissue, which is affected by severe chronic pathogenesis, is an elastic, fairly strong, elastic and smooth formation. Cartilage covers all surfaces of articulating bones: femur, tibia, patella. Thanks to the unique coating, unhindered, smooth, silent interaction of the ends of the articular bones occurs, causing the joint to move. Hyaline cartilage also serves as a shock absorber and stabilizer of movement. Due to lack of nutrition caused by negative pathological external or internal causes, it begins to gradually break down and, as a result, thin out and die.
As gonarthrosis progresses, the bone surfaces forming the knee joint become exposed and the space (articular space) between them narrows. As a result, spiky bone growths and cystic formations grow at the ends of the interacting bones, and critical deformation of the joint develops, which entails serious movement disorders. The flexion-extension potential of the lower limb in this section becomes limited, and with each stage the amplitude of movements progressively decreases. As a result, a person is unable to move normally and perform various types of physical activity, even the simplest. Stiffness of the knee is always accompanied by painful sensations, which at the initial stage of the pathology are not very disturbing, but starting from stage 2, they rapidly gain momentum in intensity.
Since hyaline cartilage does not have its own blood-vascular network, the destroyed areas are no longer restored. In a word, degenerative-dystrophic pathogenesis is irreversible in nature, and therefore it is impossible to completely cure it. But it can still be stopped in the early stages or significantly slowed down using conservative methods, preventing gonarthrosis from completely ruining a person’s quality of life. Advanced pathogenesis is treated exclusively through surgery to replace the joint with an endoprosthesis. That is why experts urge people to contact them in a timely manner: at the earliest manifestation of discomfort in the form of morning stiffness or local pain after long physical activity.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
How to treat arthrosis of the knee joint?
The level of modern medicine is at a fairly high level, which ensures successful treatment of various types of diseases. Osteoarthritis of the knees is no exception.
Today, there are a large number of methods for treating arthrosis of the knee joint.
At the initial stages of pathology development, predominantly conservative treatment methods are used. Conservative therapy includes:
- physiotherapeutic procedures;
- physical therapy (physical therapy);
- visiting various massages.
Progressive methods of treating osteoarthritis of the knee joint are also actively used. Among the modern effective ways to combat dangerous pathologies are the following:
- Ozone therapy is a local effect of ozone on the affected joint tissues. Helps reduce pain and stop inflammatory processes. Improves blood circulation in the problem area;
- kinesitherapy is a set of exercises for arthrosis of the knee joint, aimed at increasing its mobility and increasing blood flow.
Treatment of knee arthrosis with physiotherapy
Physiotherapy is one of the most popular methods of treating knee osteoarthritis.
Methods of physical influence, subject to a certain number of conditions, have the most positive effect on the area of localization of pathologies of various types.
Physiotherapy includes procedures such as:
- electrophoresis;
- ultraphonophoresis;
- irradiation with laser/infrared radiation;
- pulsed magnetic therapy.
The effectiveness of the procedures is individual and depends on the quality of the patient’s basic treatment plan.
Massage as a treatment for osteoarthritis of the knee joint
Massage is a useful addition to the treatment strategy for knee arthrosis.
Most experts around the world are of the opinion that massage is a mandatory component of the treatment of symptoms of arthrosis of the knee joint, which has a beneficial effect on metabolic processes and helps speed up recovery.
Knee massage can be performed both at home and within the walls of a hospital. The main thing during massage is preliminary high-quality warming up of the joint and compliance with the optimal duration of the process (from 10-15 minutes).
Treatment of osteoarthritis of the knee joint with massage should include techniques such as stroking, rubbing and kneading.
Gymnastics and exercise therapy for arthrosis of the knee joint
Exercises for arthrosis of the knee joint are an effective way to eliminate unpleasant symptoms and treat the disease.
The process of treating knee arthrosis is a rather complex and lengthy process, and physical therapy is an excellent assistant in achieving the desired result.
The type of exercise therapy and exercises for arthrosis of the knee joint are selected by a specialist individually, depending on the degree of development of the pathology and the general state of the patient’s physical fitness.
The main principle of gymnastics for arthrosis of the knee joint sounds like this: no increased loads on the affected joint, only rational, calm actions.
Stage 3 treatment
At stage 3 of arthrosis, surgery is performed; we will explain further why. Changes in the joint are very pronounced; at this phase, the disease extremely reduces the patient’s standard of living and performance. Osteochondral damage has reached a critical point at which the tissues of the bone junction do not represent any functional significance. The hyaline cover is almost completely destroyed. It is worth noting that this was one of the main structures of the knee, which in a healthy state was responsible for the coordinated and painless work of this part of the limb.
- Important cartilage does not repair itself, including through non-surgical methods.
- The exposed and flattened surfaces of the interacting bone ends exert unnatural pressure on each other, constantly rubbing against each other, seriously injuring nearby soft tissues and becoming even more deformed every day.
- The person feels terrible pain, not to mention the lost ability to walk normally. Patients experience daily torment, when sleep is not a joy, and during the day there is no rest from pain. Only a few people report a relatively tolerable condition.
- Anti-inflammatory analgesic drugs, as a rule, have a mild effect, but more often than not “work”. There is no point in using chondroprotectors, since strengthening and nourishing the scanty remnants of cartilage does not save the situation.
Sometimes they try to treat the consequences of grade 2-3 arthrosis with minimally invasive surgery (arthroscopy), during which marginal osteophytes can be removed, as well as torn osteochondral fragments can be removed from the joint cavity. Such manipulations, as evidenced by reviews, somewhat alleviate the patient’s condition and slightly improve motor function, but temporarily. Osteoarthritis in the knee joint remains active and will manifest itself again in the near future. Note that at 3 tbsp. Doctors mostly do not resort to minimally invasive approaches.
And this is an astroscope view of completely healthy surfaces, they are perfectly smooth.
Pathogenesis of 3-4 degrees is a very serious problem, which can only be solved with much more complex reconstructive and plastic surgical tactics. Domestic and foreign orthopedic surgeons unanimously agree that today there is no procedure that can be compared with endoprosthetics. Replacing the knee joint with a prosthesis that completely replicates the mechanical features, configuration of shapes and sizes of a natural organ will make it possible to say goodbye to both the ill-fated pathology and the disability with which it has “awarded” you.
The disease progresses quickly and can reach from the moderate-medium phase to stage 4 in a matter of months. Surgery should be performed as early as possible, before degenerative processes penetrate deep into the bone. Severely damaged bones can make it difficult to place an endoprosthesis.
Many, not fully realizing that the severity of the degenerations that have occurred are incomparable with conservative and unconventional tactics, try in every way to bypass the operation, swallowing pills by the handful, applying ointments to the sore area. Someone turns to osteopaths, private doctors who practice all kinds of alternative techniques. Unfortunately, you can’t go against nature, healing won’t come after them, and you need to come to terms with this fact. Therefore, discard senseless ideas and act prudently.
Very often the disease can develop at lightning speed.
Your physical fitness depends entirely on your decision! You can continue to suffer from stiffness and pain for life, vainly testing “empty” methods of treatment: drugs and non-standard remedies that have no evidence of effectiveness for your severity of illness. Or you can undergo surgical treatment and begin to live a full life, free from past suffering and support devices.
If you are young and only have one part of your joint damaged, a less traumatic procedure called partial joint replacement may be recommended.
There is no need to worry about surgical intervention; modern technologies have stepped far forward, and today knee joints are brilliantly replaced abroad with long-lasting implants. After such implantation, carried out in a good clinic, the risk of complications is minimal (1-2%), and restoration of mobility functions occurs in more than 95% of cases. After joint replacement, a rehabilitation course of 3-4 months will follow, including:
- physical recovery through special therapeutic exercises;
- taking medications (antibiotics, antithrombotics, etc.);
- a physiotherapy program including myostimulating, anti-inflammatory, analgesic and wound healing procedures;
- massage sessions (in the later stages of rehabilitation).
Good to know! At stage 1, the disease can be stopped and prevented conservatively. If you do nothing and start arthrosis of the knee, allowing it to move from stage 1 to stage 2, drug treatment will be much more problematic, but for a certain category of patients a non-surgical approach is still appropriate. The last two stages are always an operation.
Drugs for the treatment of osteoarthritis of the knee joint
Drug treatment for arthrosis of the knee joint is used to relieve symptoms such as pain and swelling, as well as to activate regenerative processes.
Drugs for the treatment of arthrosis of the knee joint can come in different forms (ointments/gels, tablets or injections, patches).
IMPORTANT! Any medication must be prescribed by a specialist as part of an existing treatment plan developed taking into account the symptoms of knee arthrosis.
Self-medication is unacceptable and can lead to extremely negative consequences, in particular, paralysis of the lower limbs and disability.
Painkillers for arthrosis of the knee joint
Used to eliminate symptoms of arthrosis of the knee joint.
Painkillers play an important role in the treatment of arthrosis of the knee joint, because their use improves the patient’s well-being and gives him the opportunity to get a good night’s rest.
Relief of pain is achieved through the action of active substances. The most effective tablets for pain in arthrosis of the knee joint are considered to be “Ketanol” and “Nimesulide”.
Antispasmodics for osteoarthritis of the knee
Prescribed as active assistance. A key area of focus is the fight against spasms.
The active substances included in the preparations help relax the muscle frame and provide pain relief.
Among the frequently prescribed ones, it is worth highlighting Mydocalm.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Treatment of arthrosis of the knee joint with drugs of this type not only eliminates pain, but also slows down and completely eliminates the progress of pathological processes.
Regular use of medications allows you to observe a constant concentration of active components, which guarantees a positive effect.
Artradol is considered to be the most effective NSAID.
Chondroprotectors for arthrosis of the knee joint
The main assistants in the treatment of arthrosis of the knee joint are chonroprotectors.
The active effect of chondroprotectors for arthrosis of the knee joint is aimed at restoring motor ability, which is due to the microelements included in the composition, which are an integral component in the process of building cartilage tissue.
The peculiarity of the principle of action of drugs involves a rather long, but at the same time effective process of getting rid of osteoarthritis of the knee joint.
Among the most effective and affordable drugs, it is worth highlighting Artracam, Structum and Chondroxide.
Drug treatment of arthrosis
The main role in the fight against the manifestations of gonarthrosis is played by non-steroidal anti-inflammatory drugs and chondroprotectors.
- Non-steroidal – relieve inflammation and eliminate pain. However, if you take them for a very long time, the symptoms of the disease are “masked” and it becomes impossible to prescribe adequate treatment. In addition, according to recent studies, drugs of this particular group negatively affect the synthesis of proteoglycans, which is why the affected cartilage is destroyed even faster.
- Chondroprotectors – nourish and restore the functioning of cartilage tissue. At the third stage, these medications can no longer help - they are not able to restore completely destroyed cartilage or return the knees to their original shape.
The positive effect of treatment with chondroprotectors occurs only after 6-18 months
- Medicinal ointments and creams only alleviate the patient’s condition.
- Compresses have an anti-inflammatory and analgesic effect, but, like ointments, they are only an adjuvant in the treatment of osteoarthritis and arthrosis.
Diet and general nutritional recommendations for arthrosis of the knee joint
A diet for arthrosis of the knee joint is necessary for patients with excess body weight. A low calorie diet and a wealth of nutrients will ensure weight loss and accelerate the recovery process of affected joints.
Nutrition for arthrosis of the knee joint should first of all be balanced. The daily diet should contain dishes enriched with beneficial vitamins and microelements necessary for the regeneration of joint tissues and maintaining the balance of the entire body.
It is recommended to give up not only bad habits (alcohol abuse and smoking), but also such dishes as:
- store-bought semi-finished products;
- fatty, spicy and overly salty foods;
- sweet carbonated drinks.
For convenience and competent planning of the diet, when treating knee arthrosis, it is recommended to keep a food diary, which disciplines and helps facilitate the process of restructuring the usual lifestyle.
Clinical manifestation of arthrosis of the hip joint
At the stage of the inception of the clinical picture of the pathology, the first symptoms of arthrosis of the hip joint are painful sensations in the pelvic area that occur after physical stress. The pain can radiate to the groin area and knee, becoming especially pronounced when walking. After a few seconds or minutes, the intensity of the pain decreases, and after a while it increases again. Subsequently, painful sensations are observed at rest, especially at night. In the absence of conservative treatment, the patient soon develops the chroma typical of arthrosis of the hip joint and the need to use a cane or even a walker.
Kinds
Depending on the cause of the disease, primary and secondary arthrosis are distinguished. In the first case, the pathology occurs independently against the background of the complex influence of predisposing factors. The secondary form is a consequence of other diseases and is divided into the following groups:
- joint damage resulting from metabolic disorders or endocrine diseases (gout, diabetes mellitus, acromegaly, hyperparathyroidism);
- destruction associated with congenital pathologies (Paget's disease, congenital hip dislocation, scoliosis, hemophilia, etc.);
- post-traumatic arthrosis, which arose against the background of fractures, cracks, necrotic processes or surgical operations, as well as due to the characteristics of the profession.
The most popular classification of osteoarthritis is depending on the location of the pathological process:
- gonarthrosis: damage to the knee, one of the varieties of which is palletofemoral arthrosis - destruction of the joint between the femur and the patella);
- arthrosis of the ankle joint: occurs against the background of heavy load and frequent injuries;
- arthrosis of the foot joints: the big toe most often suffers at the junction with the foot; the lesion develops against the background of gout or hallux valgus;
- shoulder arthrosis is characterized by damage to the shoulder and often occurs at a young age against the background of increased physical activity (loaders, athletes, construction workers);
- coxarthrosis: damage to the hip joint; can be both unilateral and bilateral and is one of the common causes of disability in people over 50 years of age;
- vertebral arthrosis: destruction of the cartilage discs between the vertebrae, most often affecting the cervical and lumbar spine;
- arthrosis of the joints of the hand: the joints of the fingers are most often affected; women in menopause are especially susceptible to pathology;
- arthrosis of the temporomandibular joint: it is quite rare, most often against the background of chronic inflammation due to malocclusion or improper prosthetics;
- Arthrosis of the elbow joint: a rare form of the disease, most often associated with injuries to this area.
In what cases are NSAIDs prescribed?
If the patient does not respond to paracetamol therapy, the next drug of choice is a non-steroidal anti-inflammatory drug. This medicine not only relieves pain, but also has anti-inflammatory activity. Therefore, it is preferred for synovitis, when the presence of fluid inside the joint increases the pain syndrome.
NSAIDs are the most commonly prescribed medications in the world. Every year, doctors write about 500 million prescriptions for them. 30 million people receive them every day – and these are the most conservative estimates. More than half are elderly and older people. It is not surprising that non-steroidal drugs cause a number of complications associated with the cardiovascular system and gastrointestinal tract. Therefore, self-administration of medications, especially in uncontrolled dosages, is extremely dangerous.
Ibuprofen is an effective but not safe pain reliever
Symptoms and diagnosis
Stage 1 osteoarthritis of the knee has very mild symptoms that need to be treated very carefully.
- Inconvenience when moving, especially if the discomfort occurs in one joint.
- After physical activity, mild pain and even barely noticeable swelling appear. It is important to understand that this is not pain in the literal sense, but simply some inconvenience.
- Sometimes a slight crunch in the knee is added to the uncomfortable movements.
- Fatigue sets in faster than before.
People with similar symptoms are patients of a rheumatologist. To diagnose grade 1 osteoarthritis, he uses x-rays. The photographs show a slight narrowing of the joint plane and swelling of the joint capsule. After diagnosis, the doctor selects treatment in accordance with the severity of the disease.
Treatment methods and prevention
If, after undergoing diagnostic procedures, a specialist confirms the diagnosis, you need to tune in to long-term therapy. At the first stage of the development of the disease, conservative treatment is most often prescribed - taking medications, undergoing physical procedures. It is not recommended to use any medications on your own to alleviate your condition. Only with strict adherence to medical instructions and all instructions will the treatment be successful.
The treatment regimen in each specific case is prescribed individually. This is due to the stage of development of the disease, the severity of clinical manifestations, and the presence of concomitant pathologies.
Treatment at the Energy of Health clinic
Medical orthopedists invite everyone to check the condition of the joints and, if necessary, begin treatment. We use modern effective techniques:
- full-fledged drug therapy in accordance with indications;
- physiotherapy, exercise therapy and massage;
- diagnostic and therapeutic punctures of the joint with the introduction of a synovial fluid substitute or medications;
- drug blockades for complete pain relief and other techniques.
You can view the full list of services on the website or by phone.