Video
- Heel spur. Question answer. Topic: Questions and Answers
- Heel spur Topic: Encyclopedia of diseases
Title
- Causes of the disease
- Symptoms
- Diagnostics
- Treatment methods for heel spurs
SHOCK WAVE THERAPY is the most effective method of treating HEAL Spurs!
More details
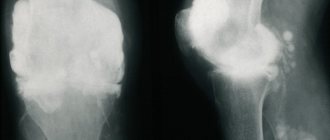
A heel spur is a deposit of calcium on the bottom of the heel bone. On an x-ray, the heel spur may protrude forward by 0.5-1 cm. Although heel spurs are often painless, they can nevertheless cause quite severe pain. Heel spurs are often associated with plantar fasciitis. Plantar fasciitis is the most common cause of pain in the lower heel. Approximately 2 million patients in the United States are treated for plantar fasciitis each year. Plantar fasciitis occurs when the strong band of tissue that supports the arch of the foot (plantar fascia) becomes irritated and inflamed. Heel spurs on the back of the heel are also often associated with inflammation of the Achilles tendon (tendinitis) and can cause tenderness and pain in the back of the heel that worsens with straightening of the foot.
Heel spurs and plantar fasciitis can occur on their own or be caused by the presence of diseases such as arthritis (including Reiter's reactive arthritis), ankylosing spondylitis, diffuse idiopathic hyperostosis. It is important to note that a heel spur may not cause any symptoms at all, and may be discovered incidentally during an x-ray examination.
Causes of heel spurs
Heel spurs are caused by:
- obesity (increased load on the legs);
- drooping of the internal longitudinal arch of the foot (longitudinal flatfoot);
- daily long standing with bare feet on a hard surface, walking on it;
- high tone of the calf muscles;
- circulatory disorders of the lower extremities;
- arthrosis, arthritis, ankylosing spondylitis;
- metabolic disorders (for example, gout);
- traumatic injury to the calcaneus.
Statistics show that in 90% of cases, heel spurs are a consequence of flat feet. This is explained by the fact that when the arch drops, the load on the foot is distributed unevenly, the tendons are constantly overstrained. It is even possible for them to be torn off from the underlying bones. As a result, not only the surface layer of bone tissue becomes inflamed, but also its deeper layers.
Prevention
Preventive measures in this case include the following:
- Timely treatment of all orthopedic diseases: diseases of the spinal column, flat feet, etc.
- Increased attention to the condition of the joints, preventing their diseases.
- Choosing the right shoes - without high heels, with a stable last, but not too flat.
- Supplementing shoes with special insoles, which are selected with the participation of an orthopedist.
- Moderate physical activity for the harmonious development of muscles, ligaments and joints.
- Elimination of foot overloads and injuries of various types (avoidance of dangerous situations).
- Regular foot exercises.
- Weight control. Excess weight puts significant stress on the heel area, which can contribute to the development of spurs.
- Proper nutrition with enough nutrients.
It is worth adhering to these recommendations at a young age in order to eliminate the risks of developing the disease in the future or to delay the first signs of a heel spur much further in time.
Symptoms of heel spurs
The size of the heel spur that occurs is not related to the severity of the symptoms of the disease. Sometimes the patient loses his ability to work with a growth of a tiny size or, on the contrary, does not experience any discomfort with a huge bone growth.
Most often, the disease manifests itself as pain while walking. The patient complains that he has a hot nail in his heel. This symptom is especially pronounced during the start of walking (after a long rest, night sleep).
Gradually, the patient's gait changes. This is due to the desire to reduce pain in the foot. Adaptive tension in the muscles of the back and legs occurs, the knees are overloaded, and the lower back and neck constantly hurt.
In some cases, the pain symptom is so severe that the person cannot step on the affected leg at all and moves on crutches.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Treatment
Nowadays, different types of treatment for heel spurs are used:
- Medication. It is aimed at relieving inflammation and eliminating pain while walking.
- MBST therapy. Used to relieve swelling, relieve pain, and improve vascular function.
- Laser therapy. Used to stimulate tissue, reduce swelling, eliminate inflammation and also relieve pain.
- Phonophoresis. The method combines the capabilities of hormonal anti-inflammatory ointment and ultrasound. Under the influence of the latter, the active substance of the ointment penetrates inside the heel more effectively and relieves inflammation very efficiently.
- X-ray therapy. During this method, the nerve endings near the heel spur are blocked - due to this, pain when walking decreases or disappears.
- Shock wave therapy. It allows the growth to dissolve. This is a non-surgical treatment that is often similar in effectiveness to surgery. True, a course of procedures will be required to achieve results.
Not all of the methods listed above always work, and therefore there remains one more option: treatment of heel spurs with surgical intervention. Typically, 5% of patients require this option.
An important aspect of treatment is also lifestyle changes and additional recommendations from doctors, for example:
- Wear special orthopedic insoles that reduce the load on the heel.
- Periodically do contrast foot baths and foot massage (strictly on the recommendation of your doctor).
- Therapeutic exercises for heel spurs (special gymnastics). They are needed to maintain blood vessels and muscles in good condition. Among the usual sports, people with this disease have access to cycling and swimming. Gymnastics for the feet without putting pressure on the heel is also useful.
- Diet to restore metabolism. As a rule, you need to focus on proper nutrition, eliminate excess salt and add enough clean water to your diet.
Much has been written about the symptoms and treatment of heel spurs in various sources that promote folk, home treatment. As a rule, the proposed methods are useless and simply waste the patient’s time. In more serious cases, if we are talking about compresses with aggressive solutions, you can even get a burn.
Do not experiment with treatment - sign up for the JSC Meditsina clinic in Moscow - our therapists and orthopedists are ready to offer you real treatment after a thorough examination. A disease such as heel spur can always be overcome with due attention and an integrated approach.
Diagnosis of heel spurs
When examining a painful heel, the doctor usually sees no changes. Calluses and swelling are only occasionally observed. When pressing on the foot, the patient experiences severe pain.
To confirm a preliminary diagnosis of a heel spur, an x-ray is taken. It shows a bone outgrowth that resembles a spike running along the plantar surface of the heel bone and exits the zone of fixation of the plantar aponeurosis. In the early stages of the disease, an x-ray may not show the presence of a spur, which makes diagnosis difficult.
It should be noted that bone growth is not always a disease. In some people, it is discovered by chance during a routine examination and does not cause any discomfort. This suggests that a heel spur may be a normal variant that does not require treatment.
Causes of osteophytes
Osteophytes form on bones in cases where the joints require compensatory support. If a joint is unable to perform its shock-absorbing function due to benign wear and tear or chronic diseases, the edges of the bones begin to touch and rub against each other. This leads to irritation of the periosteum (periosteum). Since the periosteum plays a huge role in the blood supply (and therefore nutrition) of the surface layers of bone, they begin to experience nutritional deficiencies and become vulnerable to mechanical abrasion. The periosteum also participates in the processes of bone tissue formation (it is thanks to it that the so-called callus grows on injured areas of the bone). The combination of these two factors (a decrease in bone strength and irritation of the areas that are responsible for its growth) results in the formation of osteophytes - first in the form of tubercles or small protrusions. Subsequently, they can take almost any form - a spike, a hook, a visor and others.
Cause the development of osteophytes
can:
- degenerative-dystrophic processes and diseases of bone and cartilage tissue
; - injuries
(not only bones and joint capsule, but also ligaments and soft tissues near the joint); - metabolic and endocrine diseases
(diabetes mellitus, gout, rickets); - congenital and acquired curvatures of posture and feet
(scoliosis, lordosis, kyphosis, flat feet); - inflammatory diseases of bone tissue
(tuberculosis bone infection, brucellosis); - autoimmune diseases
(rheumatoid arthritis, psoriasis); - unnaturally high load on the joints
(excess weight, professional and amateur sports, professions associated with physical labor, shifting the center of gravity during pregnancy); - oncological diseases
(both tumors with primary localization in the bone and metastases of other neoplasms).
The risk of osteophyte formation is increased by genetic predisposition, bad habits and poor environmental conditions. The progression of the problem can be affected by any factor that directly affects bone strength (for example, hormonal imbalances, stress, age-related changes, physical inactivity).
Most often, osteophytes are observed in older people, but the onset of the pathological process often occurs at the age of 40 years. Therefore, starting from this milestone, you should begin to prevent the problem and eliminate its possible causes
.
Inflammation of bone tissue
Acute and chronic inflammatory processes in bone tissue, periosteum and even adjacent articular structures (for example, tendonitis, fasciitis) can provoke the growth of osteophytes at almost any point in the affected joint. The inflammatory process is usually caused by infections (tuberculosis, osteomyelitis, brucellosis, borreliosis) and autoimmune diseases (rheumatoid arthritis, psoriasis). Patients with sources of chronic infection in the body are at risk. Inflammatory diseases of the joints are also common due to complicated infections of the genitourinary organs (gonorrhea, syphilis), intestines (salmonellosis, yersiniosis), and less often - the respiratory system (pneumonia and others).
The inflammatory process is characterized by a chaotic arrangement of osteophytes in those places where the infectious pathogen has most damaged the joints - this is how its picture differs from the degenerative-dystrophic one (in this case, osteophytes are formed on those surfaces that are most susceptible to wear and tear).
Degenerative processes in bone tissue
The most common degenerative diseases of articular cartilage and bone tissue are osteoarthritis, osteochondrosis and spondylosis. In deforming arthrosis, osteophytes can appear as an independent phenomenon without bone degradation. Most often they are observed at the edges of the articular surfaces (so-called marginal osteophytes). Despite the preservation of the bone, the growths should be treated as early as possible: over time, they can become so massive that they almost completely close the lumen of the joint space. This problem is called joint fusion and can only be treated surgically. In some cases, removal of massive osteophytes is impossible, so the joint is completely replaced (if osteophytes have grown on the vertebrae, their arches are removed).
Bone fracture
When an untreated or improperly healed bone fracture occurs, the load on the joint is distributed incorrectly. This leads to “misalignment”, in which one side of the articular surface wears out more and more and begins to become overgrown with osteophytes. Another scenario for the development of pathology is also possible: with severe or splintered bone injuries, a tear of the periosteum is possible. In this case, she begins to ossify
and
become overgrown with osteophytes
,
calcification
(calcification)
of the tendons
. Not only fractures and cracks, but also severe bruises of the periosteum and dislocations can provoke the development of osteophytes.
It does not matter how long ago the injury was received - the process of formation of osteophytes can be delayed in time for many years and even decades
.
That is why it is so important to promptly contact a traumatologist even with a severe bruise
- an unattended crack or even a microcrack in the bone, unsuccessful scarring of internal tears and other pathologies that “go away on their own”
can cause long-term asymptomatic dystrophy
.
The elbow and knee joints are especially susceptible to the formation of such post-traumatic osteophytes, and the hip joints are a little less common.
Prolonged stay in a forced position
Staying in an awkward position may be due to an unergonomic workspace or sleeping area. Incorrect body position from an anatomical point of view leads to increased muscle tone and destruction. This worsens the shock-absorbing properties of the muscle corset. Excessive physical exertion, which occurs when maintaining an uncomfortable position for a long time, causes the muscles to contract strongly, thereby injuring the periosteum and leading to microscopic ruptures of the bone capsule. The normal innervation and trophism of some areas is also disrupted due to compression of nerve endings and blood vessels. The combination of these factors forces the body to adapt and protect the periosteum in places where it is exposed to atypical loads. Since excess loads contribute to accelerated wear of synovial cartilage, the problem is complemented by a degenerative-dystrophic process - and the growth of osteophytes accelerates.
It should be noted that athletes, office workers, painters and masons, and salespeople often face the problem of staying in a forced position for a long time. Osteophytes of this kind occur in the lower back, hand joints, hip joints, calcaneal tubercle, knees, ankles, elbows and spine.
Staying in one position for a long time is a common cause of osteophytes.
Tumor diseases of bone tissue
Osteophytes can occur as a consequence of both benign and malignant tumors. Benign formations more often provoke the formation of the so-called. spongy osteophytes designed to protect synovial cartilage where its growth is impaired. In malignant tumors, osteophytes often take on the appearance of spurs and visors.
When malignant tumors metastasize (especially to the vertebral body), a severe form of osteophytes
- dense lumps occupy a large area and are difficult to treat.
Endocrine diseases
Diseases of the endocrine system (hypo- and hyperthyroidism, acromegaly), hormonal imbalances (for example, ovarian dysfunction) and age-related hormonal changes (after menopause) also have a negative impact on the human skeletal system. Osteophytes often occur as a result of neurogenic factors (stress, depression, psycho-emotional stress) or long-term use of hormonal drugs (especially with self-medication and incorrect dosage selection).
Exostoses of the ribs
The formation of growths on the ribs is more often observed with curvatures of the spine, which also lead to deformation of the chest. Their growth causes fixation of the pathological position of the chest and limitation of the vital volume of the lungs. As a result, respiratory function disorders may occur, which provokes the appearance of signs of hypoxia (oxygen starvation). To a greater extent, the lack of oxygen affects the brain, which can be accompanied by dizziness, headaches and other disorders. The heart, liver, spleen, and other internal organs are also sensitive to changes in the gas composition of the blood.
Surgery to remove exostosis
Surgical intervention is indicated for:
- large size of osteochondroma and the presence of persistent pain;
- development of complications (tendinitis, bursitis, vascular, neurological disorders, etc.);
- bone deformations as a result of the growth of exostosis;
- fracture of the base leg;
- malignancy of the tumor.
For children with bone exostosis, surgery is prescribed only in extreme cases. As a rule, it is carried out only if the testimony remains after reaching adulthood.
But if there are contraindications, surgery is not performed. This:
- purulent-inflammatory processes in the area of the upcoming intervention;
- exacerbation of chronic diseases;
- decompensated form of diabetes mellitus;
- acute infectious diseases.
Treatment of exostosis with surgery involves its complete excision with capture of the cartilaginous cap. There are several methods for removing osteochondral growth. A specific one is selected based on the location of the osteochondroma and its size. Usually preference is given to marginal resection of the growth, i.e., its removal within healthy tissue. Only in some cases is it necessary to resort to corrective osteotomy with concomitant resection of osteochondroma, but the cost of removing exostosis in this way is higher, since the operation also corrects bone deformation.
After surgery, complete recovery is observed in 98% of cases. Therefore, almost everyone who has once removed an exostosis forgets about it forever.
Marginal resection is a relatively simple type of surgery. Its essence is to expose the affected bone and remove the entire neoplasm in the front of healthy tissue along with the surrounding capsule using a sharp chisel, drill, oscillating saw or bur. After removal of the pathological formation, curettage of the maternal bone is performed using cutters and bur. In some cases, the extent of resection can be large and create the need for bone grafting using autografts or special implants. It is important to remove the entire cartilaginous cap and neoplasm, otherwise a relapse may develop.
Carrying out a corrective osteotomy involves cutting the mother's bone using an osteotome and removing the osteochondroma. After this, the bone fragments are fixed in the desired position using special plates, screws or knitting needles.
Types of osteomas
Depending on the origin of osteomas, there are:
- Heteroplastic
- formed from connective tissue. This includes osteophytes. They are found not only on bones, but in soft tissues and organs - in the diaphragm, tendon attachment points, lining of the heart, etc. - Hyperplastic
- formed from bone tissue. This group includes osteoid osteomas and osteomas.
Let's look at the subspecies that belong to two main groups.
1) Internal and external osteophytes
.
- The internal ones are called “enostoses”, they grow into the bone marrow canal. Usually solitary, except for osteopoikilosis. They do not produce symptoms and are usually discovered incidentally when a person has an x-ray.
- External ones are called “exostoses”. They grow on the surface of the bones and can appear for no reason or due to certain pathological processes. Causeless exostoses usually appear on the bones of the skull, facial and pelvic bones. They may not cause symptoms and may only be an aesthetic defect or put pressure on neighboring organs. In some cases, a fracture of the exostosis leg occurs and bone deformation occurs.
2) Osteoma
– does not differ in structure from bone tissue, usually found on the facial and cranial bones, including the paranasal sinuses. Bone osteoma is diagnosed twice as often in men, in the area of the facial bones – three times more often. These are almost always single tumors, but with Gardner's disease multiple tumors can grow on long bones. They are painless and do not cause symptoms, but when adjacent structures are compressed, various symptoms appear. Separately, there are multiple congenital osteomas of the cranial bones, which are combined with other developmental defects.
3) Osteoid osteoma
– highly differentiated bone tumor. However, it has a different structure - it consists of vascular-rich elements of osteogenic tissue, zones of bone tissue destruction, and bone beams. Usually there is no pain 1 cm in diameter. It is a common disease, accounting for approximately 12% of all benign bone tumors.
Rehabilitation
After removal of the exostosis, the patient remains in the hospital for 3 days, the sutures are removed on days 7-10. Performing marginal resection does not require any serious restrictions even in the early postoperative period. The patient can completely return to his usual lifestyle after the stitches are removed, and forget about exostosis immediately after the operation.
When performing a corrective osteotomy, complete bone fusion occurs after 6 weeks, but full recovery may require up to 3 months. At this time, it is important to strictly follow all the doctor’s recommendations and not to overload the operated part of the body. All patients who have undergone osteotomy are prescribed drug therapy, exercise therapy, and often physical therapy. The duration of rehabilitation in such cases depends on the type of surgical intervention performed and the individual characteristics of the patient.
Thus, osteochondroma is a very common type of tumor. At the same time, statistics on the frequency of its occurrence are not entirely objective, since exostoses often do not appear throughout a person’s life, and therefore are not diagnosed. However, if the formed formation bothers the patient, causes him pain, or reduces the quality of life, you should not hesitate to contact an orthopedist. A specialist will be able to assess the degree of danger of the tumor and, if necessary, remove it using the most gentle method possible.
Spinal exostosis
The lesion can occur at any level, but the thoracic region is most often affected. The neoplasm is located in the area of the arches or processes of the vertebrae. It can grow towards the vertebral or spinal canal or in an anterior direction. The first option is more dangerous, since it is capable of mechanically compressing the spinal cord and the nerve roots extending from it. This provokes the development of the so-called radicular syndrome with sharp, severe pain, radiating in accordance with the level of damage to the body part, impaired sensitivity and mobility.
Exostosis of the humerus
The humerus is one of the most common sites of osteochondroma. During its formation, the following may be observed:
- dull pain in the shoulder area that occurs when moving the arm with a large amplitude;
- a feeling of stiffness in movements, present mainly in the morning, until you manage to warm up;
- limited mobility of the upper limb in the shoulder;
- dystrophy of the muscles of the shoulder and forearm, which in difficult cases can be seen with the naked eye.
How to make an appointment with a traumatologist
JSC "Medicine" (clinic of academician Roitberg) in Moscow offers the services of qualified specialists in the field of diagnosis and treatment of osteoma. If you suspect osteoma, you can make an appointment with a traumatologist in various ways:
- select a doctor in the “Our Doctors” section and make an appointment online;
- call +7 (495) 775-73-60;
- leave a request for a call in a special form on the website.
The clinic is located in the central district of Moscow at 6 2nd Tverskoy-Yamskaya lane 10 (Tverskaya, Chekhovskaya, Mayakovskaya, Belorusskaya, Novoslobodskaya metro stations).
Exostosis in a child
It is in children that osteochondroma is most often first diagnosed, which is due to its formation from cells of the epiphyseal plate that is present only until the end of the growth period, which is adjacent to the metaphysis. It is also called the bone growth zone, since it is a hyaline cartilage whose cells are in constant miotic division. As a result, new chondrocytes (cartilaginous tissue cells) are formed, forming the epiphyseal plate, and the old ones are shifted to the metaphysis and subsequently replaced by osteoblasts (bone tissue cells).
In infants, violation of the rules for the prevention of rickets, in particular excessive use of vitamin D preparations, increases the likelihood of the formation of exostoses.
After puberty, the growth plates gradually close and are replaced by bone tissue, transforming into a thin epiphyseal line. If hormonal imbalances occur during this period, it is possible that the growth zones may remain open, which creates the preconditions for the formation of osteochondromas.
Usually, until the age of 7-8 years, bone exostosis does not manifest itself in any way in a child and makes itself felt only during the period of intensive growth, i.e., at 8-16 years, since it also begins to grow actively. In young children, such growths are present in the metaphysis area immediately near the epiphyseal plate, but subsequently move away from it and approach the diaphysis. Therefore, by how far the bone exostosis in children is from the epiphysis, the time of its formation is determined.
The growth of the neoplasm continues until the end of the growth period.