The pituitary gland is an endocrine gland located in the sella turcica (a formation in the human skull). Despite its miniature size, it controls many functions in the body. It is the pituitary gland that produces hormones that are responsible for the functioning of the entire endocrine system. Nature has reliably protected this gland from external influences, but internal factors can still cause pathological changes. One such problem is pituitary adenoma. It can be recognized by hair loss, infertility, changes in appearance, sexual dysfunction and many other signs.
Types of pituitary adenoma
There are various criteria for classifying benign pituitary tumors.
To size:
- microadenoma – tumor size up to 10 mm;
- mesoadenoma - a tumor measuring from 10 mm to 20 mm, located within the sella turcica;
- macroadenoma - a tumor measuring from 10 mm to 30 mm, or extending beyond the boundaries of the sella turcica;
- giant adenoma – a tumor larger than 30 mm.
In a simplified classification, meso- and giant adenomas are classified as medium and giant macroadenomas, respectively.
By nature of distribution:
- endosellar (intrasellar) – the tumor does not extend beyond the boundaries of the sella turcica;
- endosuprasellar - the adenoma grows upward beyond the sella turcica towards the optic chiasm;
- endolaterosellar - spread of the neoplasm into the cavernous sinuses by germination of the lateral wall of the sella turcica;
- endoinfrasellar – pituitary adenoma grows downwards from the sella turcica.
A tumor growing in different directions is called endo-supra-infra-laterosellar.
By origin:
- primary tumors;
- secondary, developed as a result of hypofunction of peripheral endocrine glands;
- adenomas caused by disruption of the hypothalamus, as well as the production of releasing hormones in ectopic formations located in non-endocrine organs.
Based on hormonal activity, pituitary adenomas are divided into active (about 60% of adenomas) and inactive (about 40%). Hormonally active tumors, based on the type of hormones they produce, are divided into:
- somatotropinomas;
- corticotropinomas;
- thyrotropinomas;
- prolactinomas.
Gonadotropinomas are also isolated, which most often do not affect hormonal levels, since they produce biologically inactive hormones. However, sometimes these tumors produce active forms of follicle-stimulating hormone and luteinizing hormone.
There are mixed tumors that produce more than one type of hormones.
Symptoms
At the onset of the disease, there are no symptoms, and the tumor, due to its very small size, is not even visible on X-ray images. In this state, the body can still eliminate it on its own, and self-healing often occurs, which the patient is not even aware of. As the tumor grows, symptoms arise, primarily associated with compression of surrounding tissues. Such manifestations of the disease include:
- migraines that are not relieved by taking medications;
- dizziness;
- double vision;
- decreased visual acuity.
Further, as the disease progresses, significant impairments in memory and speech, as well as changes in motor coordination, may occur. It is not uncommon to detect congestion of the fundus and some drooping of the eyelids. If treatment is not started in a timely manner or the tumor develops particularly rapidly, the risk of death is especially high, since the skull limits the space for growth, causing the tumor to compress the brain, injuring it in such a way that the damage becomes incompatible with life.
The patient also exhibits general symptoms, which are inherent in all malignant tumors. Such manifestations of pathology include:
- weakness;
- weight loss;
- slight drop in temperature;
- burning sensation in the area of the tumor;
- a feeling of pins and needles in the area of the tumor;
- fainting is characteristic only of cancerous formations located inside the skull.
It is important that the patient seeks medical help in a timely manner, without waiting for severe manifestations of the disease, when treatment is practically impossible.
Causes of pathology
The reasons for the development of pituitary adenoma are factors that directly affect the brain and the gland itself (trauma, neuroinfections), as well as those that have an indirect effect due to the pathology of other glands and organs. The latter include disorders of the regulatory function of the hypothalamus, thyroid gland, gonads, as well as the appearance in organs that are not endocrine glands of areas that produce hormones (for example, such accumulations of cells are found in small cell lung cancer).
In hereditary forms of the disease, mutations in suppressor genes that suppress the process of tumor cell changes play a role in the occurrence of tumors. The causes of the mutation are unknownSource: Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59.
Symptoms of pituitary adenoma
Clinical manifestations of the disease can be divided into two groups. With microadenomas or small endosellar tumors, endocrine symptoms come to the fore, varying depending on the hormones secreted.
With large hormonally inactive adenomas spreading beyond the sella turcica, neuro-ophthalmological symptoms prevail, which are different for tumors growing in different directions.
Endocrine symptoms
Somatotropinoma
A tumor that produces somatotropin, or growth hormone. Its manifestations depend on the period of tumor onset. Before the growth of bone tissue is complete (in adolescence and young adulthood), it manifests itself as symptoms of gigantism; in adults, acromegaly.
Gigantism is a proportional increase in bone length and overall height. Women can reach a height of 190 cm, men - over 2 meters.
Acromegaly is characterized by pathological growth of bones, soft tissues, cartilage, and corresponding changes in appearance - the nose, lips, chin, brow ridges, hands, feet increase disproportionately to the rest of the body. Patients experience hyperhidrosis (excessive sweating), hirsutism (excessive hair growth), severe sebum production, and the appearance of papillomas, warts, and nevi on the skin.
In addition, the patient’s internal organs become enlarged, and metabolic and endocrine processes are disrupted. From the cardiovascular system, increased blood pressure, cardiomyopathy, and cerebrovascular accidents are observed. From the nervous system - polyneuropathy, manifested by pain, paresthesia, decreased sensitivity of the peripheral parts of the extremities. The development of obesity, secondary diabetes mellitus, and thyroid pathologies is possible. Source: Main types of complications with pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92.
Corticotropinoma
A pituitary adenoma that produces ACTH is an adenocorticotropic hormone, an excess of which develops Cushing's disease. Its symptoms:
- Cushingoid obesity - an increase in the volume of adipose tissue on the face, back, hips and buttocks, and abdomen;
- swelling and congestion of the face;
- striae - stretch marks of purple-violet color on the skin of the abdomen and thighs;
- skin atrophy, especially on the back of the hands, pustular diseases, fungal infections;
- osteoporosis accompanied by multiple compression fractures;
- arterial hypertension, cardiovascular failure;
- secondary diabetes mellitus.
Thyrotropinoma
A neoplasm that produces thyroid-stimulating hormone. Thyrotropinoma can be primary or secondary.
Primary thyrotropinoma has characteristic signs of thyrotoxicosis (excess thyroid secretion). Its symptoms:
- cardiopalmus;
- tremor - trembling throughout the body, shaking fingers;
- hyperhidrosis;
- nervousness;
- bad dream.
Secondary thyrotropinoma develops as a result of a long course of uncompensated hypothyroidism. It is characterized by:
- weakness, lethargy;
- body swelling and weight gain;
- lethargy, absent-mindedness, memory impairment;
- slow metabolism.
Prolactinoma
One of the most common gland tumors. It arises from cells that synthesize the hormone prolactin. The symptoms of this pituitary adenoma are different in women and men. Source: Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L., Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80.
Among women:
- decreased sexual desire up to frigidity;
- menstrual irregularities;
- discharge from the nipples outside the period of breastfeeding;
- infertility.
For men:
- gynecomastia – enlargement of the mammary glands;
- hypoplasia of secondary sexual characteristics;
- decreased libido, erectile dysfunction;
- infertility.
Prognosis for pituitary tumors
Pituitary tumors, according to statistics, account for 15% of intracranial neoplasms. In most cases, these are benign tumors that slowly increase in size (which reduces the number of relapses); they do not extend beyond the sphenoid bone (also known as the sella turcica, where the pituitary gland is located). But there are also malignant ones, that is, those that have a cancerous nature of development.
Scientists have found that the age at which this type of disease is most often diagnosed in women and men is 30-40 years. Children very rarely suffer from this disease.
In 80% of cases, asymptomatic development of the disease is observed. It is possible to rehabilitate visual processes only at the initial stages of the development of abnormal processes.
It is difficult to make a prognosis for this disease, since it directly depends on timely recognition and initiation of treatment. Therefore, it is worth consulting a doctor promptly and undergoing routine medical examinations on time. But it is worth saying that in 25% of cases, patients with somatotropinomas and prolactinomas have a successful outcome of the disease, while the remaining adenomas are successfully cured in 80% of cases.
Gonadotropinomas
Most often hormonally inactive, they can rarely produce active forms of follicle-stimulating or luteinizing hormones, causing ovarian hyperstimulation syndrome in women.
Neuro-ophthalmological signs
With endosuprasellar adenoma, partial loss of visual fields is observed while maintaining visual acuity. An increase in tumor size leads to gradual atrophy of the optic nerves and blindness.
A tumor growing to the sides causes impaired oculomotor function (ophthalmoplegia) and double vision (diplopia), and decreased visual acuity.
When an adenoma grows into the bottom of the sella turcica, patients note nasal congestion, simulating the clinical picture of sinusitis or nasal tumors.
If the tumor grows towards the hypothalamus, patients complain of sleep disturbances, uncontrolled appetite, unstable thermoregulation (fever, chills), emotional disturbances: unstable mood, tearfulness, irritability.
With a large adenoma and its multidirectional growth, the symptoms will overlap each other and be masked. The following neurological manifestations are possible:
- headache, dizziness;
- nausea, vomiting;
- speech and facial expression disorders;
- dysphagia is a swallowing disorder.
Methods for diagnosing pituitary microadenoma
If there are primary signs of the development of a benign pituitary tumor, the patient must undergo a comprehensive examination, the main task of which is to establish the type of microadenoma and detect the factors that provoked the development of the tumor. In most Israeli clinics, the following methods for diagnosing the disease are used today:
- the patient is prescribed a comprehensive hormonal profile study;
- a complete ophthalmological examination of the patient to identify pathologies of visual function;
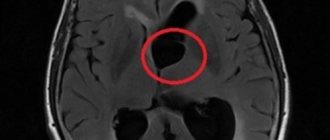
- Magnetic resonance therapy is prescribed, a procedure performed to directly visualize a pituitary tumor;
- computed tomography and x-ray examination.
A study of the patient's hormonal profile involves identifying decreased or increased levels of hormones produced by the pituitary gland. This examination helps to detect hormonally active formations, at a level with the differential diagnosis of the work of other endocrine glands of the body. Israeli doctors use the radioimmunological method for this procedure. Pituitary microadenoma
one of the first to affect the visual function of the body, therefore, in the process of diagnosing the disease, it is often necessary to resort to ophthalmological examinations. This technique allows you to determine the presence of a congestive optic disc, detect a narrowing of the visual fields, and its acuity.
Modern methods for diagnosing adenoma have become possible largely due to the availability of the necessary equipment. X-ray studies and nuclear magnetic resonance imaging make it possible to determine characteristic changes in the location of the pituitary gland and determine the infiltrative level of tumor growth. The presence of additional opportunities and means for examining the patient ensures the accuracy of the diagnosis of the disease.
Diagnosis of the disease
Patients with suspected pituitary adenoma complain to various doctors: a neurologist, ophthalmologist or endocrinologist.
At the initial appointment, the doctor will conduct a general examination, collect an anamnesis of life and illness, prescribe laboratory and instrumental tests: general blood and urine tests, blood biochemistry, ECG. A doctor of appropriate specialization will conduct an ophthalmoscopy, test visual acuity, neurological examination, and evaluate the existing symptoms.
In addition, the following studies are indicated for patients with pituitary adenoma:
- radiography of the skull;
- CT, MRI of the brain;
- Ultrasound of the thyroid gland, heart, liver, spleen;
- analysis of hormone levels in blood and saliva.
If surgical intervention is indicated, the patient must consult a neurosurgeon.
Treatment of the disease
According to clinical guidelines, there are three main approaches to the treatment of pituitary adenoma:
- conservative (medicines);
- radiation therapy;
- neurosurgical.
The drug method is indicated for small prolactin-producing adenomas. Treatment is carried out with prolactin antagonist drugs.
Radiation therapy is carried out in various ways: gamma, proton, external beam radiation therapy, stereotactic radiosurgery.
For somatotropinomas and corticotropinomas, neurosurgical removal is used. Before surgery, hormonal therapy is often prescribed to reduce the effect of hormone hypersecretion, which sometimes leads to a reduction in the size of the tumor. Drug and radiation therapy are also prescribed after surgery according to indications.
Neurosurgical intervention is recommended for macroadenomas that have severe symptoms and a risk of complications - visual impairment, up to complete blindness, hemorrhage, brain cysts. Source: Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50.
Possible complications
Microadenomas grow extremely slowly in size and cause little concern. However, the hyperplasia of their tissues gradually leads to the fact that nearby structures begin to be compressed. As a result, this can cause neurological disorders, including epilepsy and visual impairment. The pathology also manifests itself as headaches, increased blood pressure, weight changes, and decreased libido. All this negatively affects personal life and work, and as a result can lead to psychological problems. The following complications of microadenoma are dangerous:
- Cystic degeneration
. The cyst leads to frequent occurrence of severe headaches, to an unreasonable increase in blood pressure, and to mental changes. - Hemorrhage
. Its appearance is indicated by a sharp pain in the head and a sudden deterioration in vision. Hemorrhages most often occur with prolactinomas.
Hemorrhage is a dangerous complication of adenoma, but in most cases it does not lead to death. Cases of self-healing of patients after bleeding in adenoma tissue have been recorded.
Untreated advanced adenoma can lead to blindness
Timely treatment of adenomas that occur with dysfunction of the visual analyzers helps to subsequently restore vision.
[media=
https://youtu.be/ws6i6DEOOss
]
Prognosis and rehabilitation
With timely diagnosis and proper treatment, pituitary adenoma has a generally favorable prognosis without undesirable consequences. Remission after removal of an adenoma occurs in 70-80% of cases, this figure is higher for microcorticotropins and lower for somatotropins and prolactin. The relapse rate is about 12%. Postoperative mortality is low - approximately 4%, decreasing to almost 0 for endosellar and endosuprasellar tumors. The risk of mortality is higher with a large adenoma, its penetration into the ventricular system, or tumor growth of blood vessels.
Rehabilitation, as a rule, does not take much time, since most pituitary adenomas are removed transnasally (through the nose) using endoscopic instruments. In the early postoperative period, the patient is prescribed painkillers, hemostatic agents, and antibiotic therapy. If there are no complications, after a few days the patient is discharged home and is under the supervision of a doctor (ENT, ophthalmologist, endocrinologist) in the clinic. No special rehabilitation measures are required.
Prevention
There is no specific prevention of pituitary adenoma, since the exact causes of tumor development are unknown. If suspicious symptoms appear, you should immediately consult a doctor. Timely diagnosis and treatment will help achieve the most favorable results and maintain the patient’s quality of life.
Sources:
- The main types of complications from pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92
- Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59
- Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L.,
- Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80
- Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50
Contraindications to surgical treatment
Surgical treatment for pituitary adenoma is in most cases the most effective method. Based on the diagnosis, a tumor removal scheme is developed (open or endoscopic surgery with the choice of optimal access).
Contraindications to radical treatment are:
- advanced age;
- heart and kidney failure in the stage of decompensation;
- diseases of the hematopoietic organs;
- untreated infections of any location;
- post-infarction and post-stroke conditions;
- systemic diseases that occur in severe form.
If surgery is not possible, other methods are prescribed to stop the progression of the pathological process and mitigate the symptoms of the disease.